 I’m not sure what’s worse, reading the 962-page MACRA proposed ruling while in Hawaii or realizing CMS released a gigantic document that still needs to be finalized before the first surveillance year starts in just 7 short months! Instead of trying to summarize the behemoth into 500 words or less, I’ll focus in on the area that has the industry abuzz—the future of Meaningful Use (MU). (Quick hint: it didn’t really go away.)
I’m not sure what’s worse, reading the 962-page MACRA proposed ruling while in Hawaii or realizing CMS released a gigantic document that still needs to be finalized before the first surveillance year starts in just 7 short months! Instead of trying to summarize the behemoth into 500 words or less, I’ll focus in on the area that has the industry abuzz—the future of Meaningful Use (MU). (Quick hint: it didn’t really go away.)
The 101
Last Wednesday, CMS released what is known to be one of the biggest shifts from volume to value by proposing a new Quality Payment Program, a framework that will put Medicare clinicians on 1 of 2 reporting tracks: the Merit-based Incentive Payment System (MIPS) or the Alternative Payment Model (APM). These tracks were established by the latest ‘doc fix,’ the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).
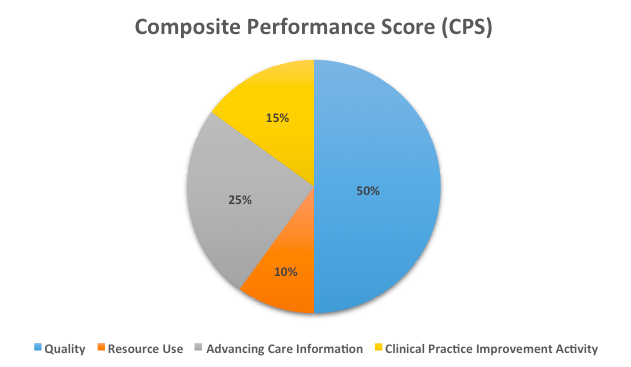
CMS predicts that a large majority of Medicare clinicians will initially participate in MIPS. Consolidating key components of PQRS, VM, and MU into a single streamlined program, MIPS evaluates performance in the following four categories:
- Quality (50% of total score in year 1): This category is pretty much our old friend PQRS, with a few adjustments. Clinicians must report on at least 6 measures with 1 being an “outcomes” measure and another being a “cross-cutting” measure.
- Clinical Practice Improvement Activities (CPIA): Allows clinicians to pick from a list of more than 90 practice goals and rewards clinical practice improvements resulting from those goals.
- Cost: Uses 40 episode-specific measures to account for differences among specialties based on claims data.
And last but not least….
- Advancing Care Information (ACI): Meet the category that will sunset the Meaningful Use program. The ACI category was designed to replace MU while still keeping certain aspects of troubled program intact. Clinicians will still report on the majority of measures listed in the Stage 3 ruling but will have more flexibility.
A clinician’s score from each category will get churned through a formula to calculate his/her Composite Performance Score (CPS). This score will be important in determining if a clinician receives a 4-9% increase or a 4-9% decrease in their year-over-year fee-for-service payment.
Diagram 1: CPS = [(quality performance category score x quality performance category weight) + (resource use performance category score x resource use performance category weight) + (CPIA performance category score x CPIA performance category weight) + (advancing care information performance category score x advancing care information performance category weight)] x 100
Similar measures, similar rules
Prior to Wednesday’s ruling, the future of MU was expected to live on within MIPS. However, after huge industry backlash and even CMS’ acting administrator saying the program was “effectively over,” we all knew something had to change. Thus, introducing the Advancing Care Information category, which will replace MU for individual Medicare-based providers (but not for hospitals or Medicaid-based providers) starting in 2017.
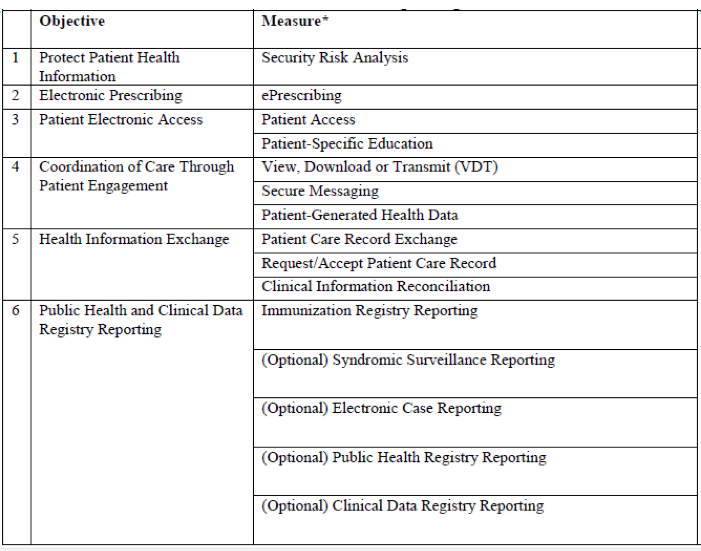
ACI will still be made up of a majority of the measures established in Stage 3 (see table below). Most of the objectives have a strong focus in the areas of patient engagement, electronic access, and information exchange. Clinicians will be required to report for a full calendar-year, but will have flexibility in determining which measures better suit their practice.
Diagram 2: Advancing Care Information objective and measure reporting
You may notice CDS and CPOE missing from the lineup. CMS is proposing to remove these 2 measures due to the fact that the median clinical performance was already extremely high under the existing MU program.
Base score and performance score
The ACI category is made up of two components—a base score and a performance score. This setup will remove the “all-or-nothing/pass-or-fail” approach of the current MU program.
Base score
The base score will reward clinicians half of the total allocated points if they simply report on all measures. Instead of needing to meet a target threshold, by just reporting a numerator for threshold-based measures or reporting a “yes” for the attestation-based measures a clinician could earn 25 points in the ACI category. However, on the flipside, failing to report all measures will result in a big fat 0 (unless the clinician qualifies for a hardship).
Performance score
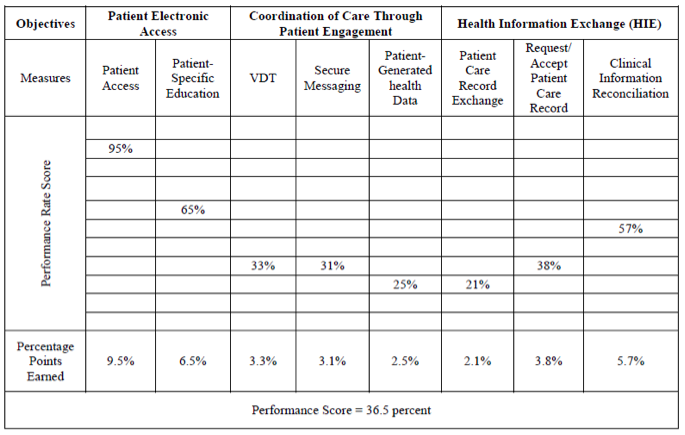
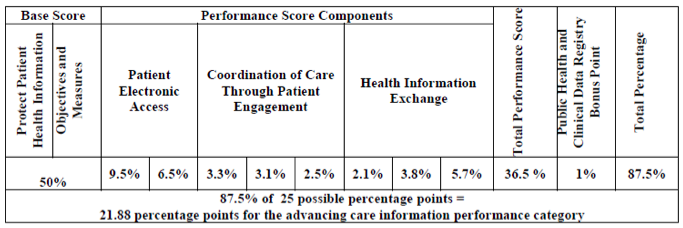
The second component of this category will score clinicians on their performance on certain measures. A MIPS-eligible clinician could earn additional points above the base score for their performance in the 8 measures that make up the following objectives: Patient Electronic Access, Coordination of Care through Patient Engagement, and Health Information Exchange.
A clinician would then take 10% of their performance rate from each of the 8 measures and the sum will be their “total performance score.” This could earn a “perfect” provider an additional 80 points.
Diagram 3: Sample performance score
Some of you may have noticed that the base score + performance score has the potential to exceed 100% within the ACI category. This was intentional. CMS hopes this methodology will allow flexibility for clinicians to focus on measures that are most relevant to their practice (and potentially achieve a maximum score for those measures) rather than focusing on achieving a “great” score for other measures that aren’t so applicable to their practice.
It doesn’t end there. Much like in high school, there is the possibility of extra credit. Clinicians can earn a bonus point by reporting to more than one public health registry.
If a clinician does earn over 100% in the ACI category, the score will get bumped back to an even 100% prior to calculating the composite performance score.
Diagram 4: Sample advancing care information performance category score
What if I quality for the MU Hardship Exemption?
As shown by recent MU attestation numbers, a majority of Nephrologists are choosing to file for a hardship exemption in the current MU program due to lack of encounters in a location with a certified EHR. If a Nephrologist continues to apply for such an exemption, CMS proposes to reweight the ACI category to zero. This would mean a clinician’s MIPS score will be totaled from the three remaining categories: Resource Use, Quality, and CPIA. I could see this posing a new set of problems!
What’s next?
For the 2016 reporting period, everything remains status quo. If you do not qualify for a MU hardship exception this year, you will have to satisfactorily meet MU for the entire calendar year in order to avoid a 2018 payment adjustment. MACRA will begin its first surveillance year in 2017 with payment adjustments starting in 2019. It is important to note that everything I covered today is still in “proposal” mode and will most likely undergo more changes before it is finalized. The public will have until June 26, 2016, to submit comments.
As Dr. Ketchersid puts it, this is no time to be asleep behind the wheel. There are many components to this ruling that will put Nephrologists in the blind spot (again). We will continue to unpack all of the twists and turns of this document on our blog in the coming weeks, so stay tuned!
 Diana Strubler, Senior Product Analyst, Health IT Standards, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Senior Product Analyst, Health IT Standards, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.




Paula Vassaur says
Thank you, Diana! This is the clearest and most concise summary I have seen so far. As always, I appreciate your posts and find them to be most helpful!