 As if the Merit-based Incentive Payment System (MIPS) wasn’t complicated enough, here I am to further complicate things! (You’re welcome!) All kidding aside, I’m going to focus on the area in MIPS that is often overlooked—reporting as a group. The decision on whether you should report as a group or as an individual under MIPS is not a simple one. There are many factors to consider. In some cases, 2 heads may not be better than one!
As if the Merit-based Incentive Payment System (MIPS) wasn’t complicated enough, here I am to further complicate things! (You’re welcome!) All kidding aside, I’m going to focus on the area in MIPS that is often overlooked—reporting as a group. The decision on whether you should report as a group or as an individual under MIPS is not a simple one. There are many factors to consider. In some cases, 2 heads may not be better than one!
What is group reporting?
CMS defines a group as 2 or more clinicians billing under the same Tax Identification Number (TIN). If you elect to report as a group, every clinician billing under that TIN must report together.
Clinicians who participate as a group will be assessed at a group level across all 4 MIPS performance categories. The group will receive one payment adjustment for the group’s performance.
There are only 2 scenarios in which an individual clinician (NPI) can be excluded from the group:
- If a clinician in a group is a qualified participant (QP) under the advanced alternative payment model (AAPM). In this scenario, this clinician’s NPI will be removed from the group prior to calculating performance. In addition, any payment adjustments that are placed on the group will not affect this individual NPI.
- If a clinician is in the first year of billing Medicare, he/she will be removed from the group prior to calculating performance. In addition, any payment adjustments that are placed on the group will not affect this individual NPI.
Here’s the kicker…if the clinician meets the low-volume threshold exemption under MIPS (bills less than $30,000 and/or sees fewer than 100 Medicare patients in a year) he/she WILL be included in the group.
What does this mean? A lot of nephrologists I work with have mid-level providers employed (especially in the dialysis units). If this practice elects to report as a group, the mid-levels will also need to participate in MIPS! That means you will need to select measures that everyone will hopefully do well in. If the mid-levels are only seeing dialysis patients, you may need to choose dialysis measures for the group.
If you are a clinician that practices under more than one TIN, you will need to meet MIPS requirements under each TIN. Reporting as a group will only cover you for that particular TIN, and only services that are provided under that TIN will be included in your group’s MIPS score.
Group scoring
Reporting as a group does not affect or change the way the MIPS composite performance score is calculated. The main difference is your entire group will have their scores averaged for each MIPS category. The average score will be the group’s score and will be compared against the MIPS threshold to determine if the group will receive any payment adjustments. If a payment adjustment is applied, it will apply to everyone under that TIN.
Submission methods
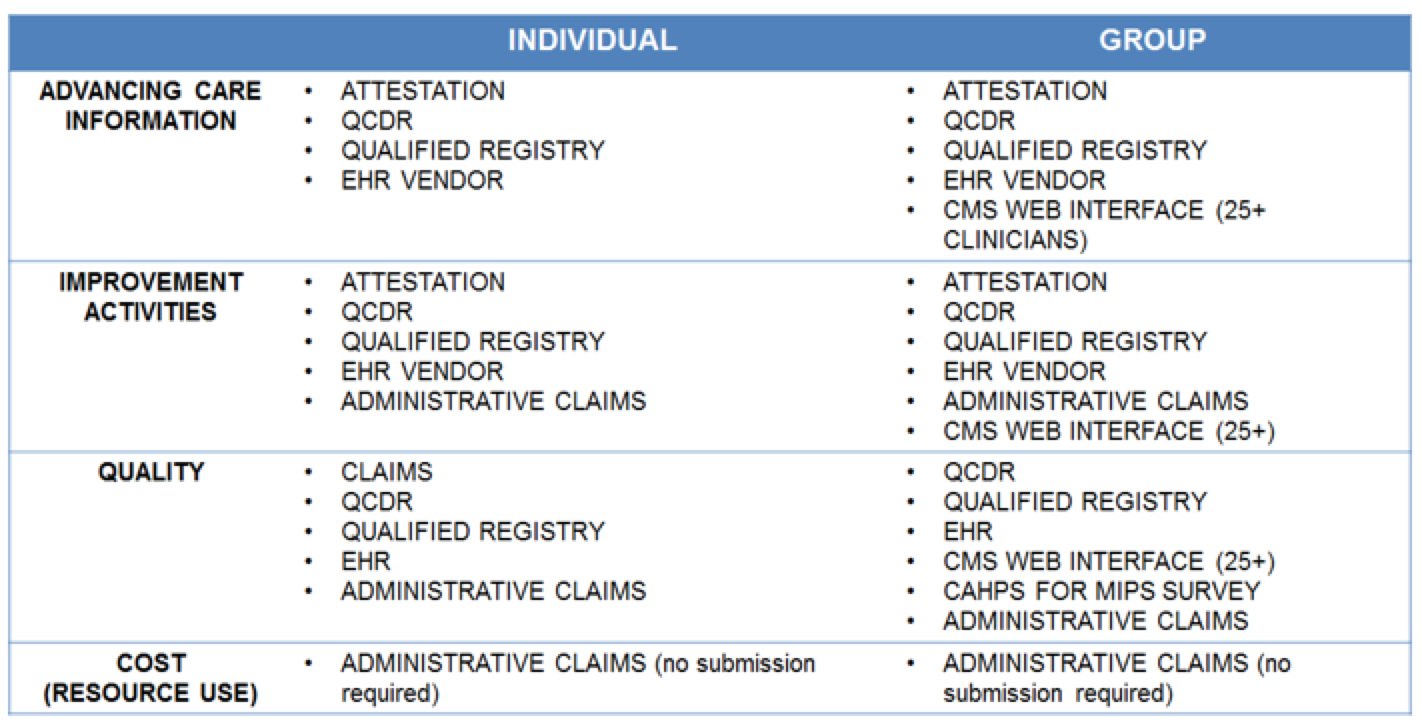
Practices that elect to report as a group will have the same submission methods available as those reporting individually (see the table below). There is no need to let CMS know that you plan to report as a group or what submission method your group will select.
The only time you will need to let CMS know that you plan on submitting as a group is if you plan on submitting your group’s MIPS data via the CMS web interface. The CMS web interface is only available for those in a group of 25+ clinicians and requires all clinicians to submit on 15 measures that CMS selected. To use this submission method, your group must register by June 30, 2017.
If your group registered as a GPRO under PQRS last year, you will automatically be signed up to report via the CMS web interface this year. If your group would like to participate through another data submission option, or not report as a group at all, you will need to “cancel” your election in the registration system by June 30, 2017.
What about those in an APM?
If you are in a MIPS Alternative Payment Model (APM), you will already be reporting as a group. The rules here are a bit different because MIPS APMs have special MIPS scoring. For example, because you are in an APM, you will be given favorable scoring in the improvement activities category.
I also want to be clear that everything I said only pertains to MIPS. If you are a qualified participant under the advanced alternative payment model (AAPM) path, you will get to avoid MIPS entirely!
To group, or not to group
Group reporting may be advantageous for some practices and probably not so advantageous for others. The best option here really needs to be determined on a case-to-case basis.
Here are a couple of examples of when reporting as a group may be advantageous:
- Group reporting is probably a good idea for clinicians who all score very similar numbers in the MIPS categories. In this case, the average score amongst all the clinicians would pretty much be the same as it would have been if they reported individually. The advantage would be less administrative time and paperwork. The person assigned to submitting the group’s data would only need to submit once on the behalf of all clinicians. It would also be easier to predict the payment adjustments across the practice (since everyone would get the same payment adjustment percentage).
- Group reporting may also be a good idea if you have some heavy hitters in your group who bring in a lot of Medicare Part B dollars, but who are struggling under MIPS. Let’s assume your practice is set up where each clinician is paid out of a pool of shared money. If you have one clinician (Dr. A) who bills $1M per year (but scores poorly in the MIPS categories), and other clinician (Dr. B) who bills $100K per year (but score extremely well in the MIPS categories), it may be advantageous to average the group’s score so that Dr. A receives a better MIPS composite performance.
Now on the flip side of case #2, if you have a lot of heavy hitters who score well under MIPS, and others who do not (such as mid-levels), reporting as a group may not be so advantageous. Instead, each clinician may want to report on their own.
To throw another wrench into things, your group payment adjustment will apply to the entire group (including new clinicians who were not in your group during the performance year). If you are thinking of growing your practice, and you received a payment adjustment as a group, that may be a big deterrent.
Every group will want to run through different scenarios to see if they should go in it together or go on their own. This decision will probably not matter so much in 2017 (since it is a transition year), but it will be something to strategize in the years ahead!
Will your practice report as individuals or as a group? We would love to hear your thoughts below!
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Image from www.canstockphoto.com




Leave a Reply