 Last weekend I spent some time with family in the cool weather of the Appalachian Mountains. While there I had the opportunity to go fly fishing. It’s important to understand that yours truly is not an avid fisherman by any stretch of the imagination, and prior to last weekend the closest I’ve been to fly fishing was watching the movie “A River Runs Through It.” Having said that, I was fortunate to be in the presence of a seasoned guide. I caught several fish in the catch-and-release stream that morning, including the one pictured in this post. In some parts of the country, I suspect the fish I caught that morning would be considered “bait.” But I must admit, while I enjoyed catching those fish, it was the act of fishing that won the day.
Last weekend I spent some time with family in the cool weather of the Appalachian Mountains. While there I had the opportunity to go fly fishing. It’s important to understand that yours truly is not an avid fisherman by any stretch of the imagination, and prior to last weekend the closest I’ve been to fly fishing was watching the movie “A River Runs Through It.” Having said that, I was fortunate to be in the presence of a seasoned guide. I caught several fish in the catch-and-release stream that morning, including the one pictured in this post. In some parts of the country, I suspect the fish I caught that morning would be considered “bait.” But I must admit, while I enjoyed catching those fish, it was the act of fishing that won the day.
A few weeks ago we discussed Alternative Payment Models (APMs) in this forum. That topic has generated quite a bit of interest, especially around the intersection of the Merit-Based Incentive Payment System (MIPS) and the APM. Within that context, I thought we would revisit the APM today. Allow me to be your guide today and with any luck you will land a “lunker” or two while we fish together.
Venn diagrams
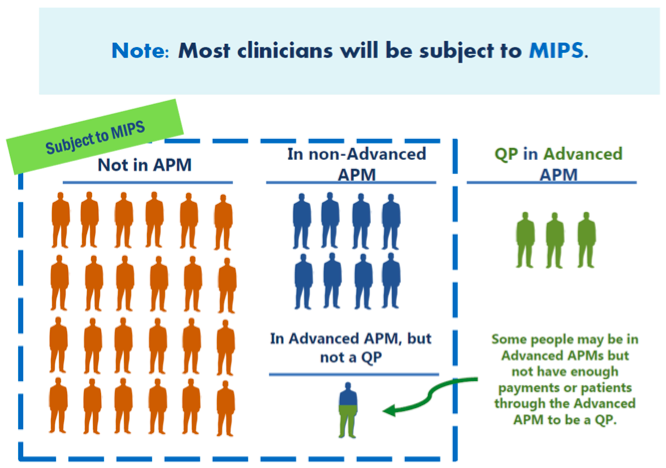
As we have mentioned before, the Center for Medicare and Medicaid Services (CMS) has put together an informative view of MACRA, which includes the image below. This image describes the intersection of APMs and MIPS.
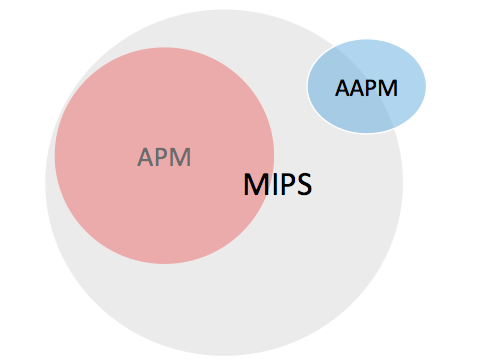
Nothing against the fine folks at the agency, but I have begun to think about MACRA, APMs, and MIPS as a collection of Venn diagrams:
The big grey beast in the middle is MIPS. The red circle completely within MIPS is the APM group. Think of these models as MIPS APMs. Perhaps the most common example is the track 1 MSSP ACO. The original rendition of the small dialysis organization ESCO lives in the red circle as well. The folks in the red circle, like track 1 MSSP ACO participants, are subject to MIPS, as are docs who do not participate in an APM.
The blue oval contains the Advanced APMs (AAPM). Included here are tracks 2 & 3 of the MSSP ACO program, along with Next Gen ACOs and the large dialysis organization ESCOs. Part of the blue oval sits in MIPS and part of it does not. If you are a participant in an Advanced APM (like an ESCO) and you clear certain targets established by MACRA, you will be designated a “qualifying participant” in the Advanced APM. That means you collect the Advanced APM financial incentive and you are excluded from MIPS. These folks are in the blue oval outside of the MIPS circle. If you are a participant in an Advanced APM and you do not clear the qualifying participant hurdles, but you come close, you are designated as a “partial qualifying participant” (Partial QP). As a Partial QP you are not eligible for the Advanced APM financial incentive, but you have the option of participating in MIPS, or avoiding it. Those folks are in the blue oval and inside the MIPS circle. Finally, it’s also possible to participate in an Advanced APM and not acheive the Partial QP status. Docs in this boat are subject to MIPS. They are also in the section of the blue oval which sits inside the grey MIPS circle.
MIPS and APMs
While the financial incentives and the opportunity to avoid the tyranny of MIPS make the Advanced APM attractive, in the early years of the program, the majority of nephrologists are not likely to have the opportunity to participate in an Advanced APM. Many participate today in a track 1 MSSP ACO. As you may recall, the track 1 program is a shared savings program, which means there is no financial downside risk. The absence of financial risk in these programs are part of what make them attractive to physicians. But the absence of downside risk is also the reason they are not in the Advanced APM blue oval above.
Assuming the bulk of what’s printed in the MACRA proposed rule makes its way into the final rule, how does your participation in an ACO impact the gauntlet known as MIPS? Remember from our earlier posts, MIPS rolls up four categories into a single number between 0 and 100. That number is your MIPS score and the MIPS score you achieve next year will determine what adjustment (up or down) CMS will make to your Part B book of business in 2019. As a brief reminder, those four categories and their year 1 relative weights are:
- Quality (50%)
- Resource Use (10%)
- Clinical Practice Improvement Activities (15%)
- Advancing Care Information, aka Meaningful Use (25%)
In an effort to reduce your reporting burden, the MACRA rule proposes to use an “APM scoring standard” for MIPS eligible clinicians participating in a MIPS APM (our red circle in the Venn diagram above). One of the first things to be aware of is the proposed rule will create an aggregate MIPS score for every eligible clinician in the APM. You read that correctly. If you are a participant in a track 1 ACO, your individual MIPS score will be identical to every other doc in the ACO and, of course, your score will in many respects depend of the collective performance of the other docs in the ACO. Make sure you choose your ACO partners well!
APM scoring for MIPS
CMS proposes to tackle MIPS scoring for docs participating in APMs in a couple of different ways. What I am describing below is the proposal for track 1 MSSP ACO participants. If your practice participates in a track 1 ACO in 2017, the quality component of your MIPS score will be derived from the performance on the ACOs quality measures which are submitted today through an existing CMS web interface. The good news here? You do not need to collect and submit separate quality data for MIPS. The potential bad news for the nephrologist? The quality component of your MIPS score is determined by the ACO’s performance on the ACO quality measures.
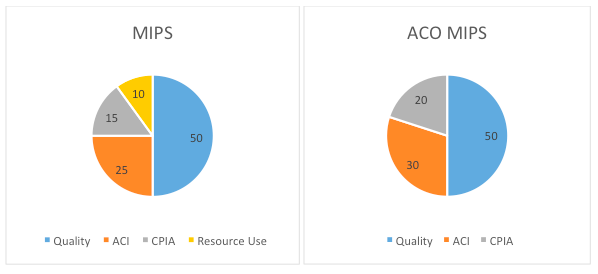
Next on the hit parade, Resource Use. APM scoring for MIPS proposes to exclude Resource Use in year 1 for APM participants. As you may recall, Resource Use is calculated by CMS using administrative claims data. In my view it is the least moveable category of the four MIPS categories. Excluding it does not help you from a reporting perspective (i.e., there’s nothing to report). What’s the impact of dropping Resource Use? Check out the pie charts below:
Quality remains the same in the chart on the right, accounting for 50% of your MIPS score. The 10 points for Resource Use are to be equally distributed between Advancing Care Information (ACI) and Clinical Practice Improvement Activities (CPIA). So the difference is a slight increase in the weight for both when compared with the standard MIPS approach displayed above on the left.
What’s the ACO impact on CPIA? By simply participating in the APM, CMS will award the ACO participants half of the maximum CPIA score. This is a nice touch, especially in the circumstance where CPIA is overweighted due to the absence of Resource Use.
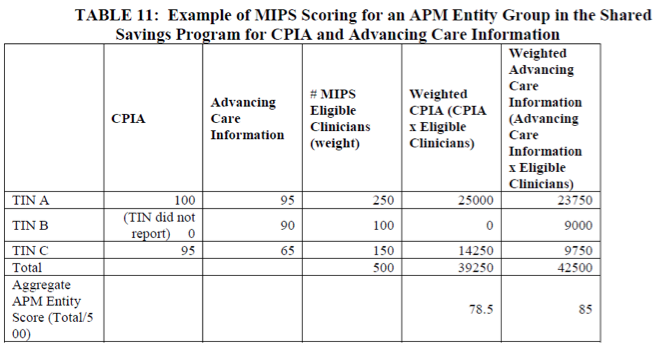
Finally, Advancing Care Information is treated the same way it is outside of an ACO. I say treated the same—and this is true from a measurement perspective—but remember you are in bed with all of the other docs in the ACO. Recall from above, your quality score for MIPS is based on the ACO’s quality performance. The same is true for CPIA and ACI. Notice the example on display in Table 11 from the MACRA proposed rule. What’s happening here is the CPIA and ACI scores for all of the ACO’s docs are rolled up in a weighted average based on the number of docs in each practice participating in the ACO, creating a MIPS composite score which is identical for every ACO participant…remember, choose your ACO carefully!
The butcher’s bill
So how did we do on this fishing trip? In my view CMS will indeed accomplish one of its goals. If you participate in an APM, your administrative overhead for MIPS will be lower. And the bump you get for CPIA is a nice touch. ACI and CPIA are slightly overweighted due to the absence of Resource Use, but the change is not significant. The surprise for me on this fishing expedition is your MIPS score will be identical to every doc participating in your ACO, and as designed, it will be dependent of your fellow ACO participants’ scores across the MIPS framework. To be clear, this is all part of a proposed rule and some of it may change.
Practices consider many things when deciding whether or not to participate in an ACO. Based on the MACRA proposed rule, one of the new things you should consider is the impact your participation will have on your 2019 Medicare Part B fee schedule. At some point before the end of this year, the MACRA final rule will emerge from the fog. If you plan to fish in the ACO stream next year, make sure you understand the MIPS implications. Remember, it’s not about the fish you catch.
Did this fishing excursion generate a question? Drop us a comment and join the conversation.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.




RG says
Brilliant explanation Terry. I appreciate it. My questions will focus on the concept if we choose to not join an ACO or an ESCO. Let’s focus on the MIPS for a 7 doctor nephrology practice (not in an ACO). Can you refresh my memory as to what the quality measures are going to be? Please provide a link as to what quality metrics we will need to report. My thinking is that we can achieve the quality outcomes better alone. Do we get a hardship exclusion for meaningful use/advancing care information if we satisfy the 50 percent rule? What can an individual group outside of an ACO do achieve the CPIA measure? What do we need to do to get a high resource utilization score, when that is finally measured later in the program? RG
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Thanks for the questions RG…some easy to answer, others not as easy. The proposed rule contained a laundry list of both existing PQRS measures as well as a number of measures which are today available via the RPA’s QCDR. There are many to choose from and you must choose 6. I’d wait until the list is finalized before I spent too much time considering the choices, but suffice it to say, there will be plenty to choose from. Importantly, with MIPS, this choice will be the most important one you make as your performance in quality (compared with the nation) will determine half of your MIPS score. You can still take the MU (or ACI) hardship exception, but realize if you do this the remaining 3 categories are over-weighted, which makes the comments above about quality all the more important. CPIA may be much easier, as small groups like yours are held to a lower standard. In my view this is the category of the 4 that is likely to see the most change in the final rule. I’d wait to see how it plays out, but as it stands today, you pick a couple of the CPIAs and attest to the fact that next year they were in play for at least 90 days. Resource Use is a crap shoot in my view. Attribution is retrospective so out of the gate you have no clue which patients have been attributed to your practice, and preventing/impacting their admissions for the reasons under study will be very difficult for you to do.
At the end of the day, it appears to me that if you have the opportunity to participate in an ESCO which will capture an appropriate percentage of your Medicare ESRD population, you are better off in the Advanced APM as opposed to independently running the MIPS gauntlet.
Best of luck,
TK