I was going to write about something other than MIPS but I truly couldn’t resist. The temptation was just too great—especially after Dr. Terry Ketchersid really shook things up with his latest blog on MIPS and the ACI hardship exception.
On top of that, since the last post, CMS has released the much anticipated quality measure benchmarks for the 2017 performance year! Now that the benchmarks are finally here, clinicians can better understand how to select their measures and somewhat predict their MIPS quality score.
What’s a benchmark?
Unlike advancing care information and improvement activities, the quality category of MIPS is determining your performance by comparing it to a national benchmark. In other words, CMS wants to know how you stack up against everyone else in the country who reported on the same measure.
In order to create benchmarks for each measure, CMS will take information that was reported via PQRS 2 years prior to the current performance year. For CAHPS, benchmarks are set based on 2 surveys: 2015 CAHPS for PQRS and CAHPS for ACOs.
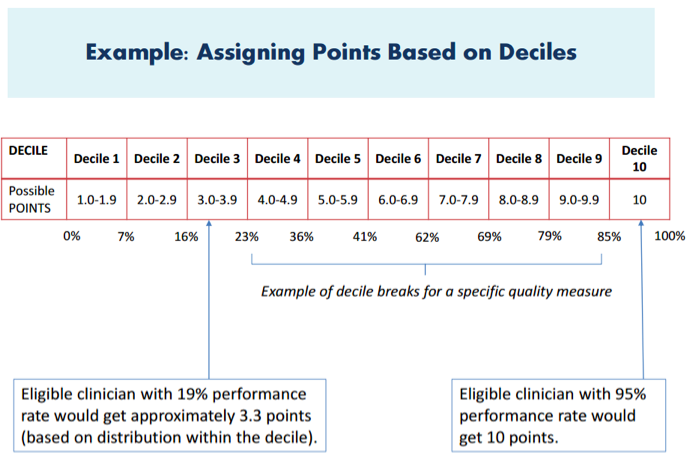
Submissions via CMS Web Interface will use benchmarks from the Medicare Shared Savings Program. CMS will then convert each measure into a 10-point scoring system. Each measure will be broken down into 10 “deciles,” with each decile reflecting one to 10 points. The deciles will be based upon stratified levels of national performance within that baseline period.
Your performance in a measure will be compared to the performance levels in the published deciles. You will receive points based upon the decile range reflecting your level of performance.
For inverse measures (like the diabetic hga1c measure), the order would be reversed. Where decile 1 starts with the highest value and decile 10 has the lowest value.
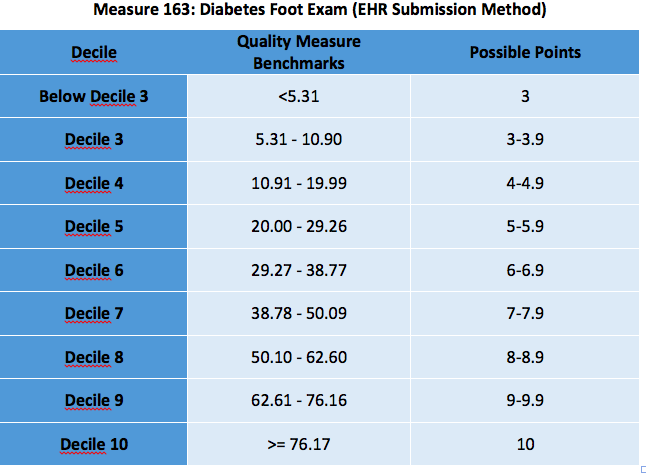
Here is an example of the Diabetes Foot Exam measure benchmarks for the 2017 performance year.
Using this example, if you submitted a performance score of 40%, you would fall within decile 7. With the tenths of deciles broken out, your points earned would likely be around 7.2. Since the decile system is a ranking method rather than a mathematical comparison, the specific ranking will not be known until the numbers have been collated in rank order.
New Measure? Buyers Beware!
Now to make matters more complicated, if you find a measure you really like, but it is a new measure (meaning it is newer than 2 years old and does not have a benchmark), CMS will attempt to calculate a benchmark based on the current year’s performance data. That means you will have no idea how well you did until after your data was submitted.
If that doesn’t bother you too much, maybe this one will: Benchmarks can only be created if at least 20 clinicians report on the same measure AND they report on a minimum of 20 patients AND they meet the data completeness criteria for that measure AND they all have greater than a 0% performance score (or less than 100% for those inverse measures).
Obviously, you will have no clue if the scenario above was met. In the case where a benchmark cannot be set (because the above criteria were not met), CMS will only award the clinician 3 points. THREE. MEASLY. POINTS. Three points are definitely enough to avoid a penalty during the 2017 transition year—but if you’re trying to earn an incentive payment, it’s not very helpful. It also not so helpful next year when the threshold is set much higher.
I have no idea why CMS made it so unattractive to report on a new measure, but I digress.
Estimating your Quality Score
Although you probably won’t be able to pinpoint the exact score you will receive for quality (prior to submitting your data), you may be able to get within a close range.
Before we get started, let’s make the following assumptions in order to keep things as uncomplicated as possible:
- You are not a part of an APM
- Clinicians in an APM (and not in the advanced APM track of the quality payment program) will have their quality score measured in different ways (depending on their APM).
- You are not in a group of 16 or more clinicians
- Clinicians in a group size of 16 or more will also be measured up against the “all-cause hospital readmission” administrative claims measure.
Step 1: To estimate your quality score, you will first have to know your performance scores for each of the six measures you selected for either a 90-day reporting period or a full year.
Step 2: Open the benchmark spreadsheet provided by CMS. On the spreadsheet, you will need to locate the measure you are reporting AND the submission type you will be choosing (EHR, QCDR/Registry/Claims).
Step 3: Look for the decile that your percentage score fell into and the number of points assigned to that decile.
Step 4: Add up all your decile points for each of the measures you are reporting.
Step 5: Add up any bonus points you may have earned. Bonus points can be earned in many different ways (included the submission type you selected and if the measure is considered high priority or an outcomes measure).
Step 6: Take the total number of points you earned and divide it by 60.
There you have it! An estimated quality score!
Bad score? Don’t fret!
Since the measure benchmark scoring concept is new, CMS finalized a measure score “floor” of three points for the 2017 performance year. That means if you just submit “something” for one measure you will earn no less than 3 points (which is enough to avoid a MIPS penalty in 2019).
Also, because this year is a transition year (and the hurdle is set so low), you don’t have to scramble to find the “right” answer immediately. Take this year to learn about all the measures that may make sense for you to report and which submission method to choose. Although some measures may look appetizing, you may not perform so well compared to others across the nation.
Isn’t pay-for-performance fun?
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.




Tara M says
Thank you for a very informative article. Would you please let me know how do I get a hold of ” the benchmark spreadsheet provided by CMS” that you refer to ? I looked all over CMS website and I cannot find that.
Your help is highly appreciated . Thank you. TM, 7/16/2017
Cheryl Burr says
Hi TM,
I found the benchmarks at qpp.cms.gov – “About” tab- “Resource Library” – “2017 Benchmarks”
Super valuable info – was very hard to find!
CB
Michelle Z says
You can find it in the QPP resource library: https://qpp.cms.gov/about/resource-library