A lot has been published about MACRA in the past weeks. The Quality Payment Program Notice of Proposed Rulemaking (NPRM) was published on April 27, 2016, and the Federal Register Proposed Rule appeared on May 9, 2016. The official title to the Proposed Rule is:
Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Incentive Under the Physician Fee Schedule, and Criteria for Physician-Focused Payment Models
By the end of last week, 3 days after publication, there were 92 public comments to the proposed rule submitted through the Federal Register site. All comments must be submitted by 5 pm on June 27, 2016, to be considered.
CMS is providing a lot of good information about MACRA and the Quality Payment Program. There is an excellent single-page CMS site that provides links to websites with webinars about MACRA and APMs. The site also links to press releases and documents about the MACRA Proposed Rule.
At this CMS site I was surprised to find some excellent slide decks about the Quality Payment Program, MIPS, and Advancing Care Information. MACRA is complicated, so the slide deck pictures are really helpful to me. For the blog post this week I’m going to post some pictures from the CMS slide deck that illustrate points Diana Strubler and Terry Ketchersid have written about in the past 2 weeks.
Eligible Clinicians
As Terry mentioned in the Acumen blog last week, “eligible professionals” are now “eligible clinicians” in MIPS and APMs, but some providers are not subject to performance adjustments as part of a Quality Payment Program. CMS graphics help make sense of who’s in and who’s out.
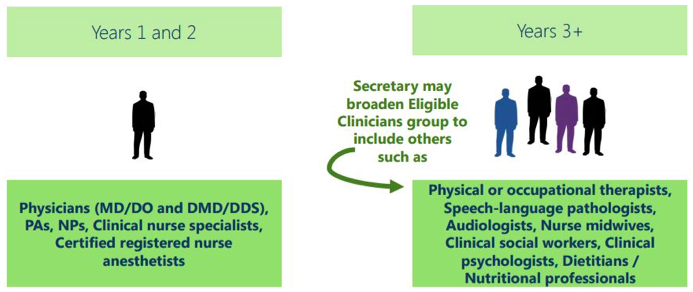
CMS Figure 1. Affected clinicians are called “MIPS eligible clinicians” and will participate in MIPS. The types of Medicare Part B eligible clinicians affected by MIPS may expand in future years.
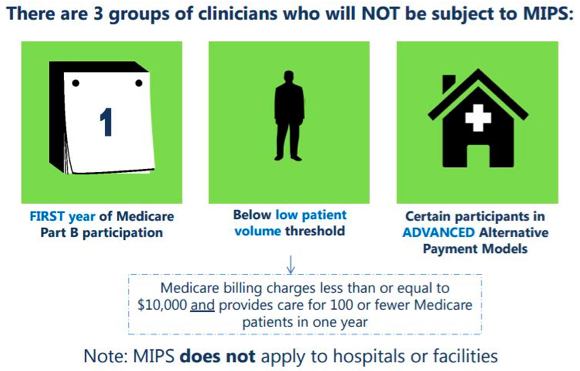
CMS Figure 2. Clinicians who are in their first year of Medicare Part B participation or below low patient volume threshold, or certain participants in Advanced Alternate Payment Models will not be subject to MIPS.
MIPS: 4 Categories of Performance
As Diana reviewed in the May 2nd blog post, participation in MIPS will involve assessment in 4 categories: Quality, Clinical Practice Improvement Activities, Cost, and Advancing Care Information. The CMS slide deck offers MIPS performance images detailing how the 4 performance categories add up to the MIPS Composite Performance Score (CPS). Quality performance is 50% of the total MIPS score in year 1 and is very similar to PQRS. CMS summary slides provide point-by-point details like this one about the MIPS Quality Performance Category:
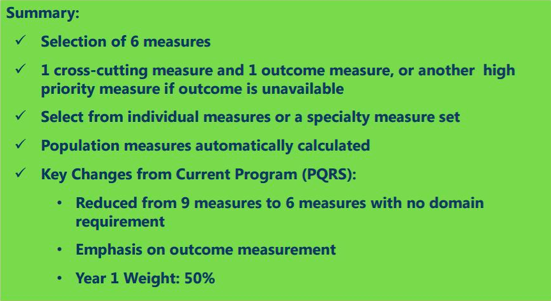
CMS Figure 3. Summary of the MIPS Quality Performance Category.
In the same post Diana provided details on the MIPS Advancing Care Information (ACI) category which has 2 parts — the base and performance scores. CMS provides images to detail the ACI base score and performance score:

CMS Figure 4. The objectives and measures for the MIPS Advancing Care Information base score.
Note that some base score objectives require on a yes/no attestation while others include reporting of numerators and denominators.
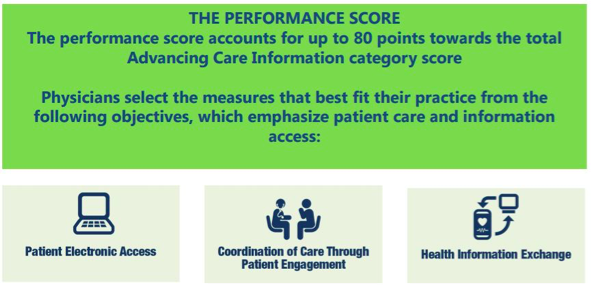
CMS Figure 5. The objectives for the MIPS Advancing Care Information performance score.
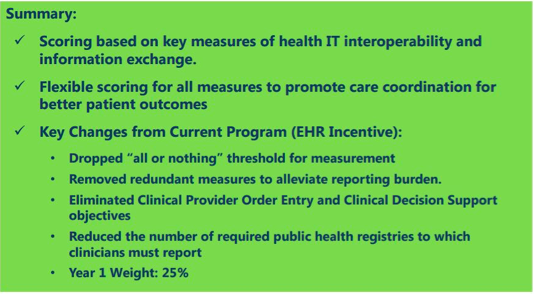
CMS Figure 6. Summary of the MIPS Advancing Care Information performance category.
As Diana noted in the early May blog post, the measurement year for MIPS is calendar year 2017, so this is the time to get ready to meet the performance measures. The CMS slide deck provides details on reporting and on the payment adjustments eligible clinicians can expect.
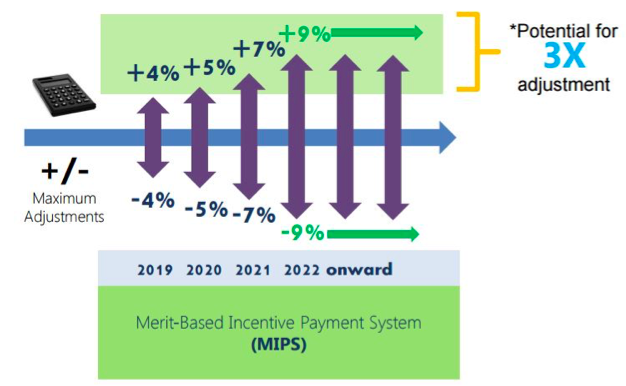
CMS Figure 7. Payment impact that will begin in 2019 based on 2017 performance.
Advanced APMs
In the Acumen blog post last week Terry provided an overview of participating in an Alternative Payment Model (APM) to avoid MIPS. The May 9th post gives key information about the 3 APM categories including the “Advanced APM”. The CMS slide deck has details and examples about meeting the criteria of an Advanced APM.
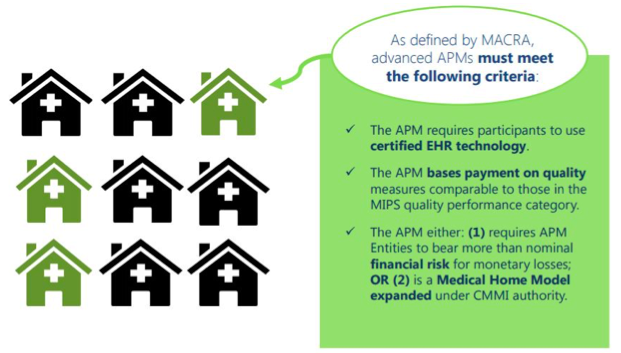
CMS Figure 8. CMS Advanced Alternative Payment Model overview.
As Terry notes, becoming a “qualifying APM participant” or “QP” in an Advanced APM is a good thing that leads to the “APM incentive”, which CMS illustrates like this:
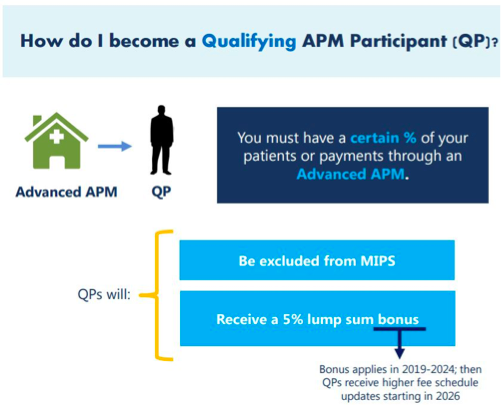
CMS Figure 9. Path to becoming a qualifying APM participant, or QP.
Information in the slide deck addresses how clinicians become QPs and how the qualifying thresholds will change over time. Mark your calendars now because here is the CMS MIPS and Advanced APM timeline:
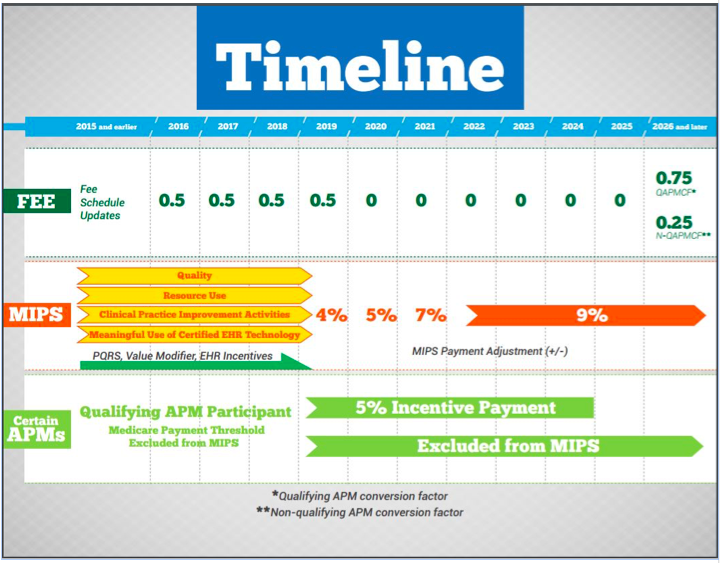
CMS Figure 10. CMS MIPS and Advanced APM timeline.
In the Acumen blog we’ll continue to keep an eye on the 962-page MACRA NPRM and the public comments submitted to the Federal Register website. Check out the helpful CMS resources including the Quality Payment Program training, MIPS training, and Advancing Care Information slide decks posted on the CMS Quality Payment Program website when you have a chance. If you have comments about MIPS or APMs to share with us, feel free to comment here!
By the way, the CMS Quality Payment program is really good, but before you hang your hat on anything, read this:
CMS Figure 11. CMS slide deck disclaimer.
 Dugan Maddux, MD, FACP, is the Vice President for CKD Initiatives for FMC-NA. Before her foray into the business side of medicine, Dr. Maddux spent 18 years practicing nephrology in Danville, Virginia. During this time, she and her husband, Dr. Frank Maddux, developed a nephrology-focused Electronic Health Record. She and Frank also developed Voice Expeditions, which features the Nephrology Oral History project, a collection of interviews of the early dialysis pioneers.
Dugan Maddux, MD, FACP, is the Vice President for CKD Initiatives for FMC-NA. Before her foray into the business side of medicine, Dr. Maddux spent 18 years practicing nephrology in Danville, Virginia. During this time, she and her husband, Dr. Frank Maddux, developed a nephrology-focused Electronic Health Record. She and Frank also developed Voice Expeditions, which features the Nephrology Oral History project, a collection of interviews of the early dialysis pioneers.




Leave a Reply