 Can you believe it? In less than 2 weeks, 2017 will be here, and with the New Year comes the biggest change to physician reimbursement our generation has seen. The newly minted Quality Payment Program, with all of its complexity, will have an impact on your future Medicare Physician Fee Schedule (PFS), and the fun begins in just 12 days. Over the past few months the Acumen blog has unpacked a number of details related to the MACRA legislation. Today, let’s have some fun with numbers.
Can you believe it? In less than 2 weeks, 2017 will be here, and with the New Year comes the biggest change to physician reimbursement our generation has seen. The newly minted Quality Payment Program, with all of its complexity, will have an impact on your future Medicare Physician Fee Schedule (PFS), and the fun begins in just 12 days. Over the past few months the Acumen blog has unpacked a number of details related to the MACRA legislation. Today, let’s have some fun with numbers.
Where’s Waldo?
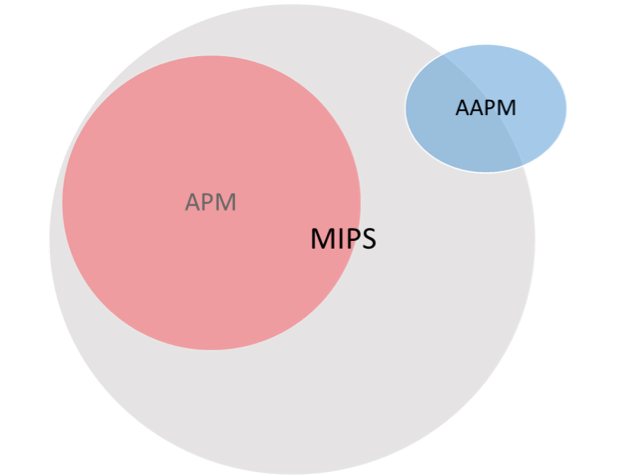
Before we dive into the numbers, here’s a brief recap. Unless you are new to Medicare, bill Medicare less than $30,000 per year, or see fewer than 100 Medicare beneficiaries each year, in 2017 you will find yourself in one of the buckets in the Venn diagram below:
Stated another way, in 2017 you will be either:
- An Advanced Alternative Payment Model (AAPM) participant—think ESCO or Next Gen ACO, among others
- A MIPS Alternative Payment Model (APM) participant—like a track 1 Medicare Shared Savings Program ACO
- A MIPS eligible clinician—by far the largest category in 2017 (i.e., every clinician who is not in the red or blue circles above)
The numbers
When Health and Human Services (HHS) responds to new legislation with large programs like this one, they are compelled to run the numbers to evaluate the impact such a program has on people like you. Buried in the back of the remarkably long MACRA final rule are the numbers used to evaluate this program’s impact. I found some of these numbers of interest, and I hope you do as well.
Practice revenue
The first number should come as no surprise. When HHS estimates the economic impact this program will have, they largely focus on practice revenue. “On average, clinicians’ Medicare billings are only about 23 percent of total revenue, so even those MIPS eligible clinicians adversely affected by MIPS would rarely face losses in excess of 3 percent of revenues,” the HHS standard for determining whether an economic effect is “significant.” Of course nephrologists would never be accused of being average! In fact, the typical nephrology practice relies on Medicare for a substantially larger share of total practice revenue, often upwards of 60-70%.
Nephrology ECs
Of additional interest, per the final rule, CMS believes there will be 11,089 MIPS eligible clinicians (ECs) in 2017 who have designated their specialty as nephrology. Unclear to me how they can be so precise, and the number seems a bit high to me, but those are topics for another day. Of note, those 11,089 ECs represent less than 1% of the total number of ECs billing Medicare for professional services. Of this 11,000+ figure, CMS believes 364 nephrology ECs will be excluded from MIPS as they will be new to Medicare. Another 263 will miss the fun because they are QPs in an Advanced APM (the blue oval in the Venn diagram), and a surprising 1,704 will be excluded because they bill less than $30k or see fewer than 100 beneficiaries.
That leaves 8,759 nephrology ECs living in the grey MIPS circle above, who in 2017 will need to run the MIPS gauntlet. Thankfully that run will be a cake walk next year due our new friend Pick Your Pace. By the way, those 8,759 nephrology ECs can be found in table 58 in the final rule where they sit among the 698,486 ECs running the MIPS gauntlet next year. That table also displays the average Part B charge per EC. There are 48 rows in that table (yes, I counted) representing every type of provider from anesthesiology to vascular surgery. The average Part B charge per nephrology EC is $249,805, which makes us the seventh-highest average among the 48 provider types listed, behind Hem/Onc, Ophthalmology, Rheumatology, Radiation Oncology, Vascular Surgery, and Dermatology.
But wait, there’s more
Last, but certainly not least, as part of this exercise HHS is compelled to zero in on the potential negative financial impact this program will have. The good news is that next year that impact is low, thanks in large part to Pick Your Pace. To evaluate the impact, they run 2 different scenarios. The first they call “Standard Participation Assumptions”, which basically means 90% of you will participate in MIPS. The second scenario is cleverly labeled “Alternative Participation Assumptions”, which assumes only 80% will choose to wade into the MIPS pool next year. The upshot? Under the 90% participation scenario, 5.7% or just over 400 nephrologists will face the MIPS penalty in 2019. With the 80% scenario, that figure jumps to 8.9% or north of 600 nephrologists. That penalty will end up costing those docs about $10,000 due to the 4% reduction in their 2019 PFS. Hard for me to believe there could be that many nephrologists out there willing to take it on the chin, particularly during the transition year, but perhaps there are still a few out there who do not read the Acumen blog!
What’s in a number?
There’s an old saying that is widely quote in the financial world, “past performance is no guarantee of future results.” All of these estimates are based on historic data and they lean heavily on the 2015 PQRS experience. Using averages is also a bit problematic in this exercise. Having said that, there are some valuable takeaways here, which we sometimes take for granted:
- We are a tiny specialty swimming in a big pond.
- Due to the high cost of care for the ESRD population, Medicare represents a substantially higher percentage of our total revenue than the typical non-nephrologist enjoys.
- And, last but not least, due to the looming ESCO expansion, the percentage of nephrologists avoiding MIPS because of their participation in an Advanced APM will substantially exceed every other specialty in medicine in 2017.
There are many ways to slice and dice this program and the numbers above represent but a small slice of the MACRA pie. As the end of the year comes to a close we hope that all of you are preparing for a successful run at the Quality Payment Program next year. In the meantime, all of us here at the Acumen blog would like to wish each of you a safe and healthy holiday season. Happy Holidays!
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Top image from www.canstockphoto.com



Leave a Reply