 How hip are you to textspeak? GM had me stumped for quite a while. I kept receiving emails that started with the greeting “GM” and I had no idea who GM was. After 50 emails it finally occurred to me that GM was the latest NetLingo for Good Morning. I haven’t told my daughter this story yet because I am anticipating an LOL from her in response.
How hip are you to textspeak? GM had me stumped for quite a while. I kept receiving emails that started with the greeting “GM” and I had no idea who GM was. After 50 emails it finally occurred to me that GM was the latest NetLingo for Good Morning. I haven’t told my daughter this story yet because I am anticipating an LOL from her in response.
According to the online Urban Dictionary “textspeak” involves shortening of words typically in a text message to make the phrase “cooler,” but I’m beginning to think health care and health IT are the super-coolest with shortened words for every concept. Test your HITLingo with these: HIE, CEHRT, FLEX-IT, MIPS, APM, ACO, ESCO, AHRQ/NQS, MACRA, and VBP. If you’re stumped like me, then here’s a refresher on the HIT Top 10.
The HIT Textspeak Top 10 (aka HTT10)
HIE: Health Information Exchange (HIE) will be a frequent flyer in your 2016 HIT inbox. HIE is the focus of HIT incentive programs including Stage 2 Meaningful Use (MU2). Information exchange is expected to increase significantly between patients and providers through patient portal use and other healthcare applications. Patients are expected to engage in reviewing medical records, communicating with providers, and accessing personal health data to share with other providers. Health IT News suggests that new applications will enable patients to access data from multiple providers to create a “mash up” of comprehensive personal health data.
CEHRT: Electronic Health Records (EHRs) must meet standards created by the Office of the National Coordinator for Health IT (ONCHIT) to become certified electronic health record technology (CEHRT). Many of the CEHRT standards are dedicated to functionality that meets MU documentation and reporting requirements. As a nephrologist you may notice that your EHR has functionality you never use, but it is required as part of the general ONC certification.
In 2015 CEHRT is an issue for nephrologists since it impacts the MU hardship exception. As Terry Ketchersid discussed in his December 14 blog post, nephrologists often experience more than half of their outpatient encounters in a dialysis facility that is not utilizing a CEHRT. Unlike the physician’s practice, the nephrologist who is not the owner or majority owner of the dialysis facility does not have direct control over the EHR decision. This allows many nephrologists to qualify for a MU exception.
FLEX-IT: This is not your New Year’s resolution fitness plan for 2016. This is the Flexibility in Health IT (FLEX-IT) Reporting Act of 2015 introduced in the U.S. House of Representatives in January of this year. This Act directs HHS to continue to use a 3-month or 90-day reporting period for EHR incentive programs this year. A CMS Final Rule was published on October 16, 2015, that confirmed a 90-day MU incentive program reporting period instead of a full calendar year.
MIPS: The Merit-based Incentive Payment System (MIPS) signals the end of a Medicare annual calculation of base reimbursement with automatic increases for physicians. Beginning in 2019 reimbursement will be tied to physician performance. MIPS unites pay-for-reporting or performance programs such as PQRS and MU to create performance metrics that generate a “MIPS score” between 0 and 100. The “MIPS score” has 4 components: MU, the resource component of the Value-based Modifier, performance measure of quality similar to PQRS, and clinical practice improvement. As Terry has discussed in earlier blog posts, MIPS will be administered at the individual provider or National Provider Identifier (NPI) level and it’s a zero-sum game. Generally the number of physicians who underperform will be similar to the number who overperform.
APM: Alternative Payment Models (APMs), as Terry suggests in his July 20 post, may save physicians from the underperformer/overperformer assessments of MIPS. If you have “significant” participation in an APM, then you are exempt from MIPS and may receive a participation bonus of 5% on your Medicare business. APMs hold physicians accountable for spending and quality. APMs also grant flexibility to design coordinated care activities that impact cost and quality. Here are common APMs:
- Accountable Care Organizations (ACOs)
- Bundled Payments for episodes of care such as the current hospital Bundled Payments for Care Improvement (BPCI)
- ESCOs
- Pay-for-Performance
- Patient-Centered Medical Homes
ACO: Accountable Care Organizations (ACOs) bring together providers, hospitals, and other community health care organizations to create integrated and coordinated services for Medicare patients. Health and Human Services (HHS) is committed to tying 30% of Medicare spending to APMs like ACOs by the end of 2016. CMS views ACOs as a way to spend healthcare dollars more wisely by holding physicians and healthcare organizations accountable for providing quality care with efficient use of resources. This is the Value = Quality/Cost equation referred to in the May 18 blog post. CMS has been encouraged by the cost savings produced by some ACOs that launched in 2012.
ESCO: ESRD Seamless Care Organizations (ESCOs) are the first disease-specific ACOs. ESCOs consist of partnerships among physicians and other pertinent providers who care for dialysis patients. An ESCO must have at least 1 nephrologist or nephrology group and at least 1 dialysis facility. A cost “baseline” is established for each ESCO entity and future performance is compared to this benchmark. Flexibility to utilize new coordinated care models within the ESCO should result in improved patient quality outcomes at a lower cost. Cost savings will be shared among the ESCO partners.
AHRQ/NQS: The Agency for Healthcare Research and Quality (AHRQ) is the HHS agency created to “produce evidence to make health care safer, higher quality, more accessible, equitable, and affordable.” AHRQ activities include funding projects to test new models of care, supporting the development of teaching and training modules for health care organizations and providers, and generating data from Medicare/Medicaid claims and patient and provider surveys. The agency plays a role in using data to influence and inform health care policy.
In 2011 AHRQ expounded on Don Berwick’s Triple Aim and established six quality priorities, which are part of the National Quality Strategy (NQS). In his March 16 blog post Terry listed the 6 NQS priorities:
- Making care safer by reducing harm caused in the delivery of care
- Ensuring that each person and family are engaged as partners in their care
- Promoting effective communication and coordination of care
- Promoting the most effective treatment and prevention practices for the leading causes of mortality starting with cardiovascular disease
- Working with communities to promote best practices to enable healthy living
- Making quality care more affordable for families, individuals, employees, and government by developing and spreading new health care delivery models
In turn these 6 NQS priorities have become the 6 NQS Domains, which are central to value-based programs like PQRS. The 6 Domains are:
- Patient Safety
- Patient and Family Engagement
- Care Coordination
- Clinical Processes/Effectiveness
- Population and Public Health
- Efficient Use of Healthcare Resources
MACRA: The Medicare Access & CHIP Reauthorization (MACRA) Act of 2015 became Public Law No: 114-10 on April 16, 2015. This Act of congress repealed the Sustainable Growth Rate (SGR) and “improved” Medicare payment for physician services, thereby modernizing the Medicare payment system. In addition, a section of the law provides a 2-year extension to the Children’s Health Insurance Program (CHIP).
This MACRA mandated a new reimbursement framework that ties reimbursement to performance, creating a value-based purchasing system for Medicare. MACRA also consolidates the quality reporting programs from individual incentive and penalties to a single quality measure, with payment through MIPS or participation in an APM.
CMS VBP: Value-based Programs and Value-based Purchasing (VBP) tie provider reimbursement to quality of care based on the “three part aim”:
- Better population health
- Better individual health
- Lower cost
Terry has written a lot about the Value Modifier (VM) Program or Physician Value-based Modifier (PVBM). The November 23 blog post describes the quality composite score created from PQRS and patient outcomes measures, which will impact 2016 Medicare payments to providers. Today the ESRD Quality Incentive Program (QIP) for dialysis facilities is a VBP. APMs and MIPS are future VBPs for everyone.
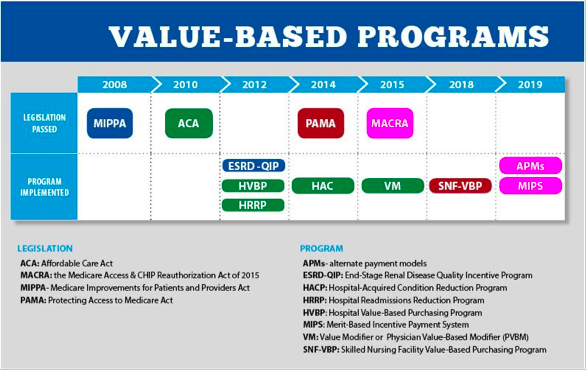
Here is the CMS timeline for legislation and implementation for VBPs:
FWIW these are the HTT10. You might be tempted to say NIMBY or TMI, but this is the new reality. Don’t H8, just stick with the Acumen Blog and GAC ASAP. It’s really NBD and you’ll do GR8!
(Here’s the translation for those like me who are not so hip to textspeak: For what it’s worth, these are the HIT Textspeak Top 10. You might be tempted to say not in my back yard or too much information, but this is the new reality. Don’t hate, just stick with the Acumen Blog and get a clue as soon as possible. It’s really no big deal and you’ll do great!)
Happy CY 2016 and TTFN!
 Dugan Maddux, MD, FACP, is the Vice President for CKD Initiatives for FMC-NA. Before her foray into the business side of medicine, Dr. Maddux spent 18 years practicing nephrology in Danville, Virginia. During this time, she and her husband, Dr. Frank Maddux, developed a nephrology-focused Electronic Health Record. She and Frank also developed Voice Expeditions, which features the Nephrology Oral History project, a collection of interviews of the early dialysis pioneers.
Dugan Maddux, MD, FACP, is the Vice President for CKD Initiatives for FMC-NA. Before her foray into the business side of medicine, Dr. Maddux spent 18 years practicing nephrology in Danville, Virginia. During this time, she and her husband, Dr. Frank Maddux, developed a nephrology-focused Electronic Health Record. She and Frank also developed Voice Expeditions, which features the Nephrology Oral History project, a collection of interviews of the early dialysis pioneers.




Leave a Reply