 Fireworks started early this year in Washington. Not only did the Senate reveal a draft of the healthcare reform plan, but the Centers for Medicare and Medicaid Services (CMS) also unveiled another highly anticipated document: the 2018 Quality Payment Program (QPP) rule.
Fireworks started early this year in Washington. Not only did the Senate reveal a draft of the healthcare reform plan, but the Centers for Medicare and Medicaid Services (CMS) also unveiled another highly anticipated document: the 2018 Quality Payment Program (QPP) rule.
This is the first rule that has been released since Trump appointed Health and Human Services Secretary Tom Price and CMS Administrator Seema Verma. Both Price and Verma have emphasized that they want to reduce reporting burdens and allow clinicians to focus on patient care. Does the 2018 proposed rule reflect that? Let’s see!
Before I begin, I must throw out the following disclaimer: These changes are meant for year 2 of the program (or the 2018 performance year). These changes are proposed and do not affect this year’s performance period.
Alright, now let’s jump in!
More clinicians excluded
One of the biggest moves in the 2018 proposed rule was increasing the low-volume threshold to allow more clinicians to be exempt from MIPS. The low-volume threshold moves to <$90,000 part B allowed charges OR <200 part B patients.
This probably doesn’t affect a large majority of nephrologists out there, but it probably does affect the mid-levels.
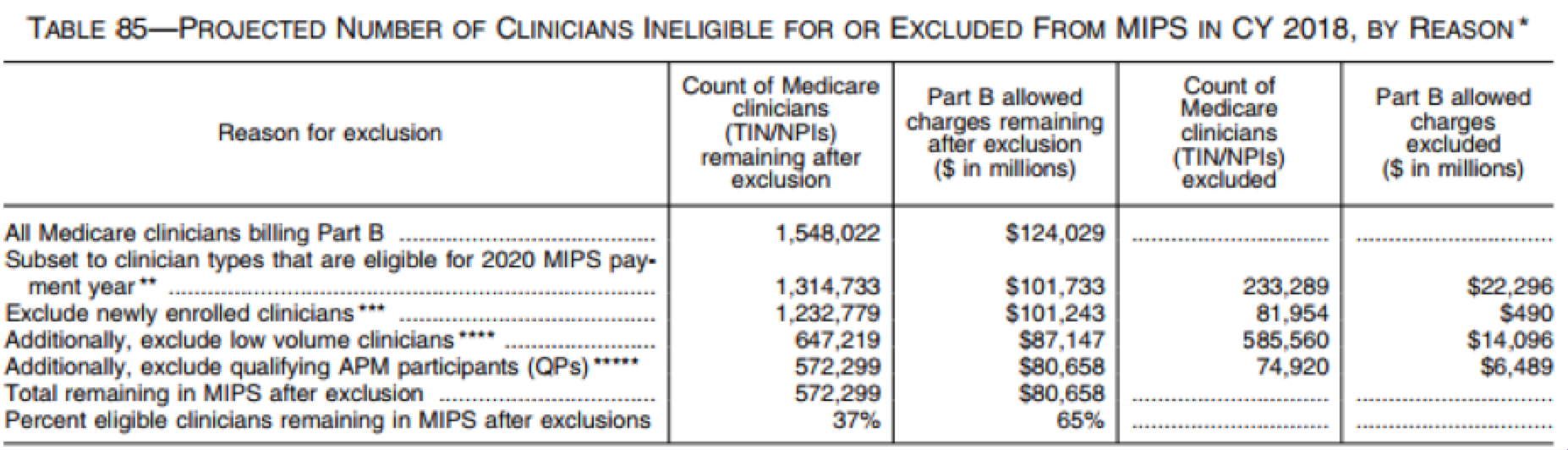
By upping the low-threshold numbers, CMS expects to exclude a total of 585,560 clinicians. This means 63% of clinicians that bill to Medicare will be exempt from MIPS. See this table from the CMS MACRA 2018 proposed rule for details:
To determine eligibility in the 2018 performance year, CMS will look at data from September 1, 2016, to August 31, 2017. If you meet the low threshold qualification, you are all set to skip MIPS. CMS will then come around a second time and look at data from September 1, 2017, to August 31, 2018, to identify additional clinicians who should be excluded. If you were excluded in the first round, you will stay excluded (even if you don’t pass the second round).
Things to consider:
- You will not be excluded from MIPS (even if you qualify as a low-volume clinician) if your practice decides to report as a group!
- This doesn’t exclude you forever! The determination will be made each performance year.
- The fee schedule is still frozen. If you are out of MIPS (and not in any risk-sharing model) you probably won’t see any type of Medicare pay increase. The only way to get paid more is to do more.
Virtual group participation option in 2018
Solo doc or small practice? CMS is allowing you to band together to create a virtual group (regardless of location or specialty). Starting in 2018, solo practitioners or groups of 10 or fewer eligible clinicians can come together “virtually” with at least one other clinician or group to participate in MIPS. The virtual group will need to meet the same measure and performance category requirements that are set for “non-virtual” group reporting.
Things to consider:
- All eligible clinicians under the TIN would be part of the virtual group (including those who may have been individually exempt due to low volume).
- Virtual groups that choose this participation option would need to make an election prior to the 2018 performance period.
Multiple submission methods per category
CMS is proposing to allow for multiple submission methods within a single MIPS category. This would allow clinicians to report using more than one reporting method (for example they can report quality data via their EHR and a registry—not just one or the other).
This one may help the clinician (allowing for more measure choices), but will probably cause practice administrators a bit of heartburn. Can you imagine keeping track?
MIPS scoring changes
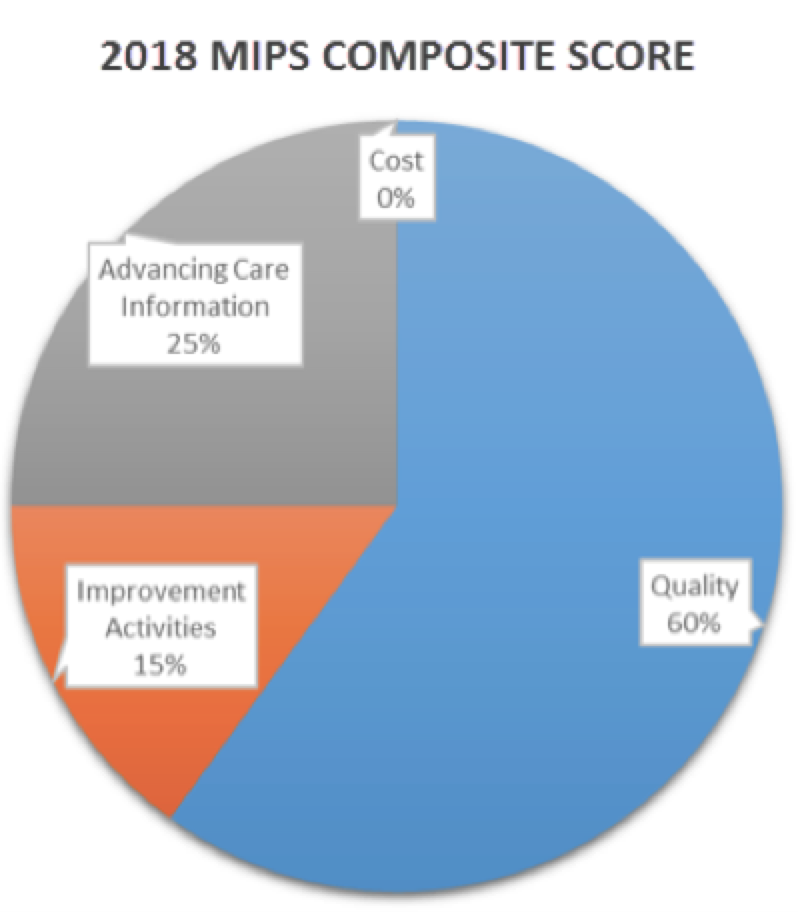
CMS is proposing to keep the weights for each category the same in 2018. Most notably, that means the “cost” category will still be set at 0% in 2018.
Although the MIPS category weights remain the same, some of the category requirements are proposed to change.
Quality category changes
We all know quality is the monster of MIPS. I was shocked (and quite disappointed) to see this category barely change. One change that nephrologists will see in the proposed rule is the creation of a nephrology specialty set. What does this mean? Not much, except that CMS is pointing out measures that may be good for a nephrologist to select.
Remember the criteria for this category:
- Will award a minimum of 3 points for all measures submitted (as long as they meet the data completeness requirements).
- Will only award 3 points for each measure submitted that does not have a benchmark. Pay close attention to this one when selecting a nephrology measure!
- Will only award 3 points for measures that do not meet case requirements.
- Will award 1 point for measures that do not meet data completeness requirements (small practices will continue to get 3 points).
- CMS will set a cap of 6 points for selecting certain topped out measures.
As always, choose your measures wisely.
Additional hardship exceptions for Advancing Care Information
To further align with the 21st Century Cures Act, clinicians who have an EHR that was decertified during the performance year can claim a hardship under Advancing Care Information (ACI). Likewise, clinicians in a small group who still do not have a certified EHR (and have good reason as to why) can also claim a hardship. Clinicians who decide to take a hardship under ACI will need to apply for one prior to December 31 of that performance year.
Things to consider:
- If you choose to take a hardship of any kind in ACI, your MIPS composite performance score will be reweighted. The 25 points assigned to ACI will now move over to quality—making quality 85% of your MIPS score! Proceed carefully!
- You will need to prove hardship every year.
Allows use of a 2014 Edition Certified EHR in 2018
Clinicians can still use their 2014 Edition Certified Electronic Health Record Technology (CEHRT) rather than be required to upgrade to 2015 Edition technology in 2018.
Because of this, CMS is extending the 90-day reporting period for ACI for both 2018 and 2019. Essentially, clinicians do not have to use a 2015 Edition EHR until October 2019.
For clinicians who do move over to a 2015 edition EHR next year, CMS will award you 10 bonus percentage points under the advancing care information performance category.
Bonus points for seeing complex patients
CMS will award between 1 to 3 bonus points for clinicians who see a more complex patient population. Complexity will be measured by using a Hierarchical Condition Category (HCC) risk score. The HCC score compares Medicare beneficiaries’ FFS spending to the overall average for the entire Medicare population. The HCC score methodology has been used in other CMS programs for risk adjustment.
CMS created this bonus opportunity for two purposes:
- To protect access to care for complex patients and provide them with excellent care; and
- To avoid placing MIPS eligible clinicians who care for complex patients at a potential disadvantage
It is safe to say, as a nephrologist you will mostly likely earn the full 3 bonus points (that will be added to your overall MIPS composite performance score). As Dr. Ketchersid mentioned last week, the proposed rule states that nephrology has the highest average HCC risk score (3.05) among all other specialties (the average is 1.08)! In other words, CMS is stating that nephrologists take care of the most complex patient population. On the flip side, dermatologists shouldn’t count on any bonus points here.
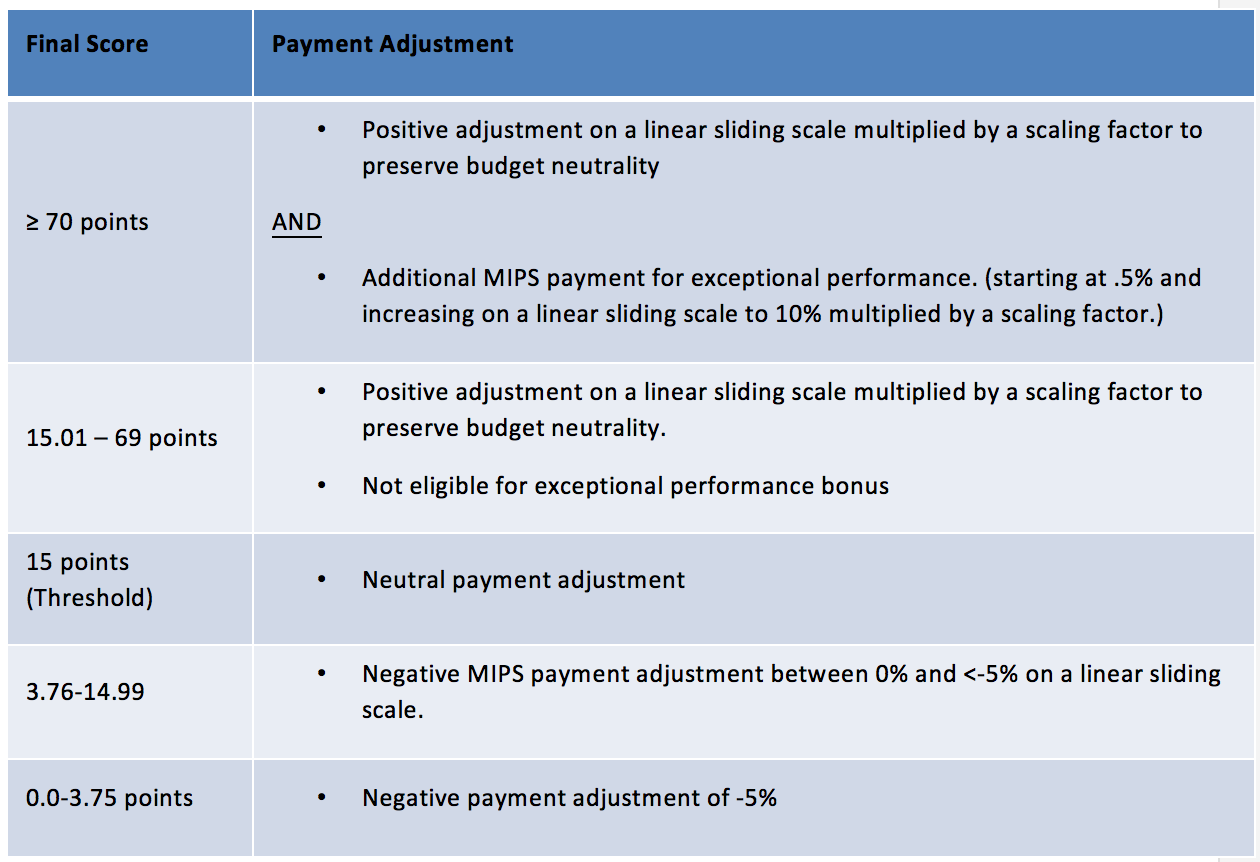
Another low MIPS threshold
To avoid a penalty in 2020, eligible clinicians will only need to earn 15 points in the 2018 performance year. CMS decided to inch up the threshold from 3 to 15. This makes it super easy (once again) to avoid a penalty. Think about it, just submitting one high-weight improvement activity already puts you over the bar!
Things to consider:
- Exceptional performance is still set at 70 points or higher.
- Because MIPS is a budget-neutral program, people must lose for others to win. A lower bar means fewer “losers” which means fewer bonus dollars.
What about the Advanced APM changes?
I am going to redirect you to last week’s blog for more on this topic. Dr. Ketchersid did a fantastic job not only covering the Advanced APM proposed changes, but he also shared some interesting facts about ESCOs!
Boom or bust?
The proposed rule largely left the structure the same (outside of some quick fixes to help the underdogs with exemption or success). It is clear that payment and delivery-system reforms are still pushing forward regardless of who is in office.
The 2018 proposed changes will most likely boost a nephrologist’s MIPS composite score, but are these changes just a band-aid?
The rule will be finalized later this fall after a 60-day comment period by the public.
What do you think of the changes? Let us know below!
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Image from www.canstockphoto.com




Roger W Coomer, MD says
How does one submit or document a “Security Risk Analysis” for MIPS?