Seema Verma, Administrator of the Centers for Medicare and Medicaid Services (CMS), recently announced that 91% participated in the first year of the Quality Payment Program (QPP), barely squeaking by their goal of 90%.
Due to these high numbers of participation one would think there’s a lot of money in the pot. Right? Well…probably not.
One man’s loss is another man’s gain
As required by the Medicare Access and CHIP Reauthorization Act of 2015, CMS must implement Merit-based Incentive Payment System (MIPS) payment adjustments in a budget-neutral manner—meaning the agency may not pay out more in incentive payments than it recoups in penalties. In other words, if there are not a lot of losers, there are not a lot of winners.
The maximum negative adjustment for the 2017 performance period is -4% for not participating. Clinicians at or above the performance threshold of 3 points earn a neutral or positive adjustment. The adjustment is applied on a linear scale, so clinicians with higher scores earn a higher adjustment.
Figure 1: MIPS 2017 Performance Year Payment Adjustment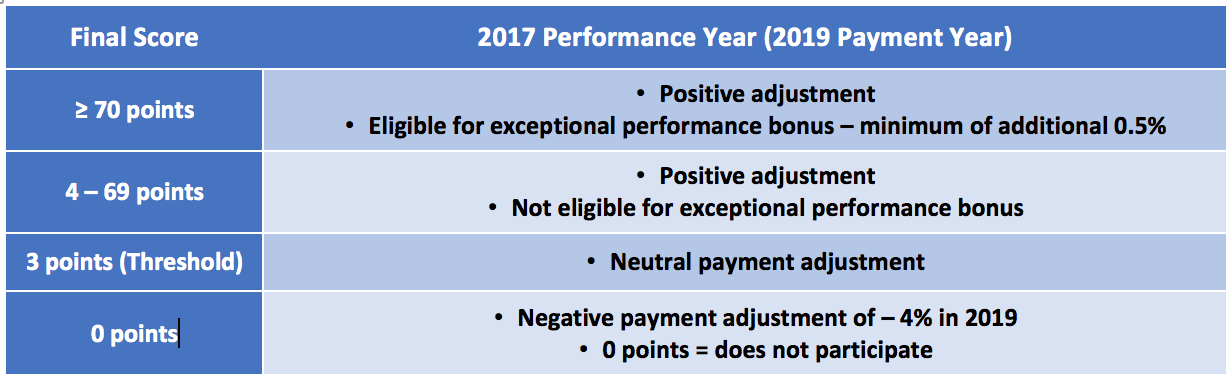
Here is where the math gets tricky. The amount of the positive adjustments is scaled and will depend on the scores as well as the total number of clinicians both above and below the performance threshold. The positive payment adjustment in 2019 for a score of 100 is established at +4% adjusted up or down by a scaling factor.
For clinicians with a final score of 100, the adjustment factor would be 4% times a scaling factor greater than 0 and less than or equal to 3.0. The scaling factor is intended to ensure budget neutrality, but cannot be higher than 3.0.
More clinicians above the performance threshold means the scaling factors would decrease because more clinicians receive a positive MIPS payment adjustment. More clinicians below the performance threshold means the scaling factors would increase because more clinicians would have negative MIPS payment adjustments and relatively fewer clinicians receive positive MIPS payment adjustments.
The image below was published in the 2017 MACRA final rule and is for illustrative purposes only. The scaling factor for the 2019 payment year will not be known until later this year.
Figure 2: Illustrative Example of MIPS Payment Adjustment Factors Based on Final Scores and Final Performance Threshold and Additional Performance Threshold for the 2019 MIPS Payment Year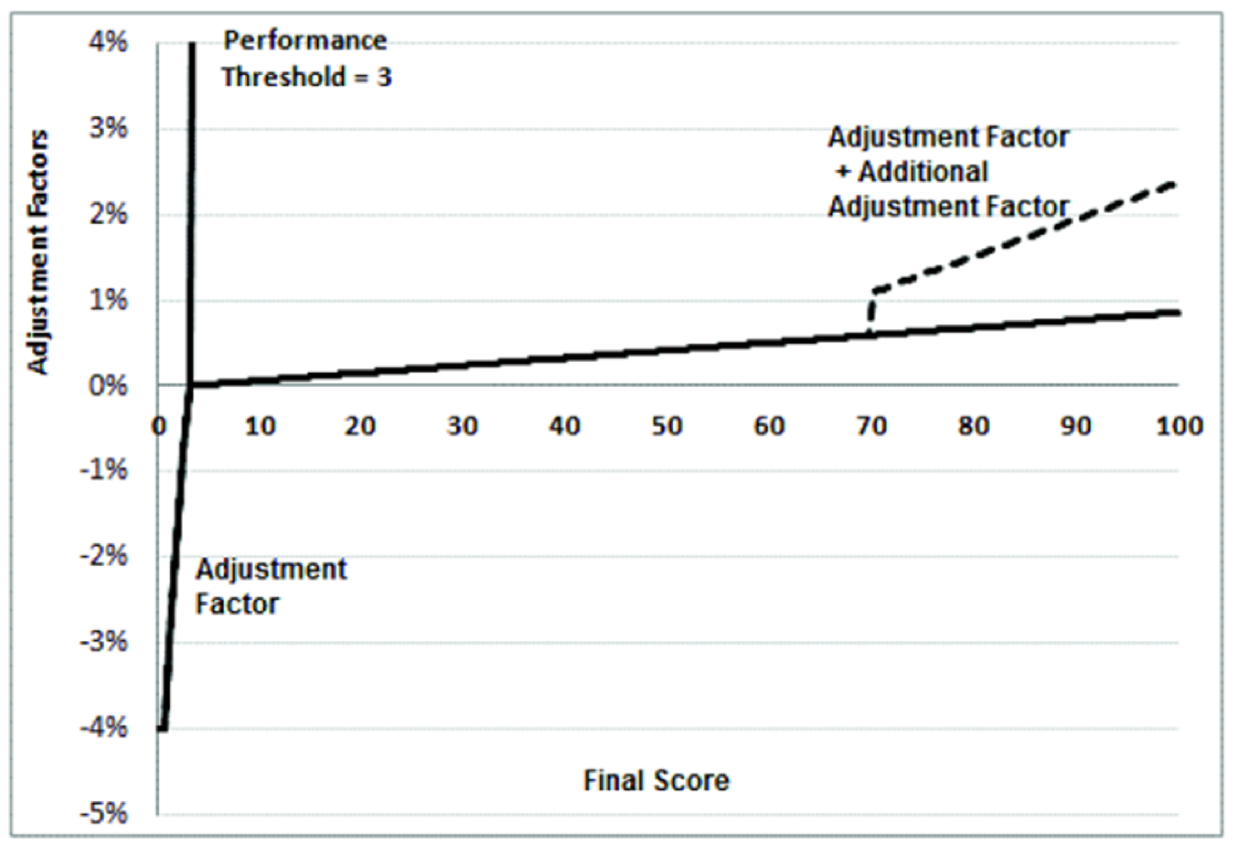
In the first year of the program, CMS anticipates that the payment adjustment for MIPS eligible clinicians with a final score of 100 points would most likely be around a +2.4% payment adjustment or less.
Which in turn means those clinicians who did well, but not perfect, will receive even less than that.
Where did the money go?
When MACRA was first proposed, clinicians were eligible for around $833 million in incentive payments under MIPS for the 2019 payment year. This assumed that around 746,000 clinicians would be required to report under the MIPS track of the QPP.
At that time, the proposed rule had set the low-volume threshold at $10K. That meant clinicians who billed Medicare Part B $10K or less per year would be exempt from the MIPS program.
This amount quickly dropped to $199 million once the low-volume threshold was finalized at $30,000 and the bar to avoid a penalty was set very low with the “pick your pace” path.
Figure 3: MIPS Estimated Payment Adjustment Pool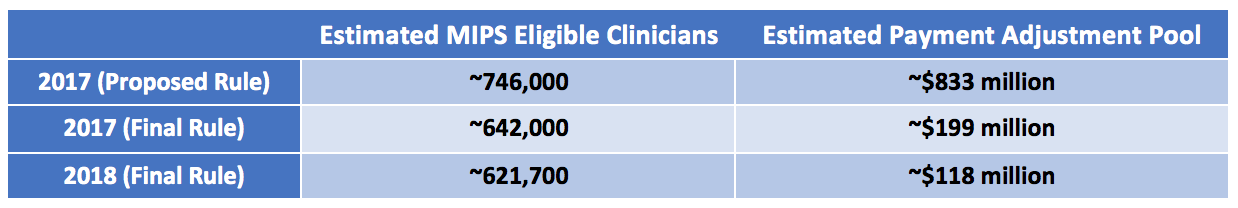
Therefore, if a MIPS consultant ever knocks on your door promising you a +5% bonus for your 2019 reporting, you should run the other way.
When the bar to lose is set low and less than 50% of clinicians are eligible to participate, the math just doesn’t work out.
The money may not be worth it, but what about your reputation?
I’m sure many of you are now thinking that the money isn’t worth the effort. Or maybe it will cost you more to report than what you will earn. These are both fair statements. However, I caution you from throwing in the towel.
By law, CMS will publicize your final MIPS score for the world to see on the Physician Compare website. Not participating could result in immeasurable negative consequences. Whether it be patients comparing physicians, payer negotiations, or seeking employment into a new practice, your MIPS score may come into play.
What is your 2017 MIPS Score?
If you submitted 2017 MIPS data through the QPP website, you can access preliminary performance score and feedback data with your Enterprise Identity Management (EIDM) credentials.
Keep in mind this score could fluctuate a little based on the following items still being reviewed:
- Special status scoring considerations
- Final calculations of the All-Cause Readmission Measure for the Quality performance category
- Inclusion of claims measures from 60-day run out period
- Results of the CAHPS for MIPS Survey
- Approval or denial of Promoting Interoperability performance category Hardship Application
- Improvement Activities Study participation and results
- Creation of performance period benchmarks for Quality measures that didn’t have a historical benchmark
If none of these items above were applicable to you, then the score you see will most likely remain the same. Your final MIPS score will be available sometime in July. Make sure you know what the final score is for all TIN/NPI combinations you are associated with!
Once your final score is set, CMS will compare you against others to see how you rank, and the pool of money will be identified then redistributed in 2019.
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.



Leave a Reply