 Can you believe it? Fall officially begins this Friday! The football season is underway, the leaves will soon change colors, and before you know it, the College Hoops season will begin! It is hard to believe 2017 will soon be coming to a close. I am in a bit of a nostalgic mood today as I recently came across two perspectives written in the New England Journal of Medicine (NEJM).1,2 Each piece was written by Health IT luminaries, and each shares somewhat opposing conclusions. Those of you expecting more MIPS and MACRA today may need to skip the blog this week. Today we are going to take a trip down memory lane.
Can you believe it? Fall officially begins this Friday! The football season is underway, the leaves will soon change colors, and before you know it, the College Hoops season will begin! It is hard to believe 2017 will soon be coming to a close. I am in a bit of a nostalgic mood today as I recently came across two perspectives written in the New England Journal of Medicine (NEJM).1,2 Each piece was written by Health IT luminaries, and each shares somewhat opposing conclusions. Those of you expecting more MIPS and MACRA today may need to skip the blog this week. Today we are going to take a trip down memory lane.
ARRA
I’ll start this story in early 2009. Remember what you were doing 8 ½ years ago? The Steelers had just won the Super Bowl, and as painful as it is for me to type this, the Tar Heels of North Carolina would soon win the NCAA Men’s college basketball tournament. I was the CMO of a tiny EHR company, laser focused on the specialty of nephrology. We were unbelievably busy because the country’s new President had recently signed into law something called the American Recovery and Reinvestment Act of 2009 (ARRA). ARRA was a massive stimulus package, created at a time when much of the country was struggling. Buried within ARRA was a relatively small piece of legislation called the Health Information Technology for Economic and Clinical Health Act. Talk about a mouthful! Thankfully someone had the clever idea to shorten that to the HITECH Act.
HITECH
In retrospect, HITECH was audacious in its aspirations. Using significant financial carrots (and later financial sticks), HITECH was overtly designed to move our country away from paper-based medical records, replacing those with the promise of electronic health records (EHRs). Gone would be the days of misplacing office charts ahead of patient visits. No longer would our nurses or staff spend countless hours on the phone asking the referring doc yet again to please fax those records for the new consult sitting in the waiting room. And, oh yes, trying to decipher your colleague’s chicken scratch would be a thing of the past. Fast forward to 2017…with upwards of $37 billion dollars of taxpayer money changing hands, have those aspirations been realized?
National Coordinators
The first of the 2 perspectives in the NEJM was authored by not 1, not 2, not 3, but 4 former National Coordinators for Health IT.1 The fact that there have been that many National Coordinators at ONC raises a few questions, but I digress. In all fairness, these folks had a very short runway. In very short order a formal framework for Meaningful Use (MU) was established. Literally hundreds of Health IT applications ran the “certification gauntlet” in order to receive the ONC Good Housekeeping Seal of Approval, a certification necessary for providers to collect their HITECH dollars. I still remember the high anxiety those alternate-year rituals created for our small software firm.
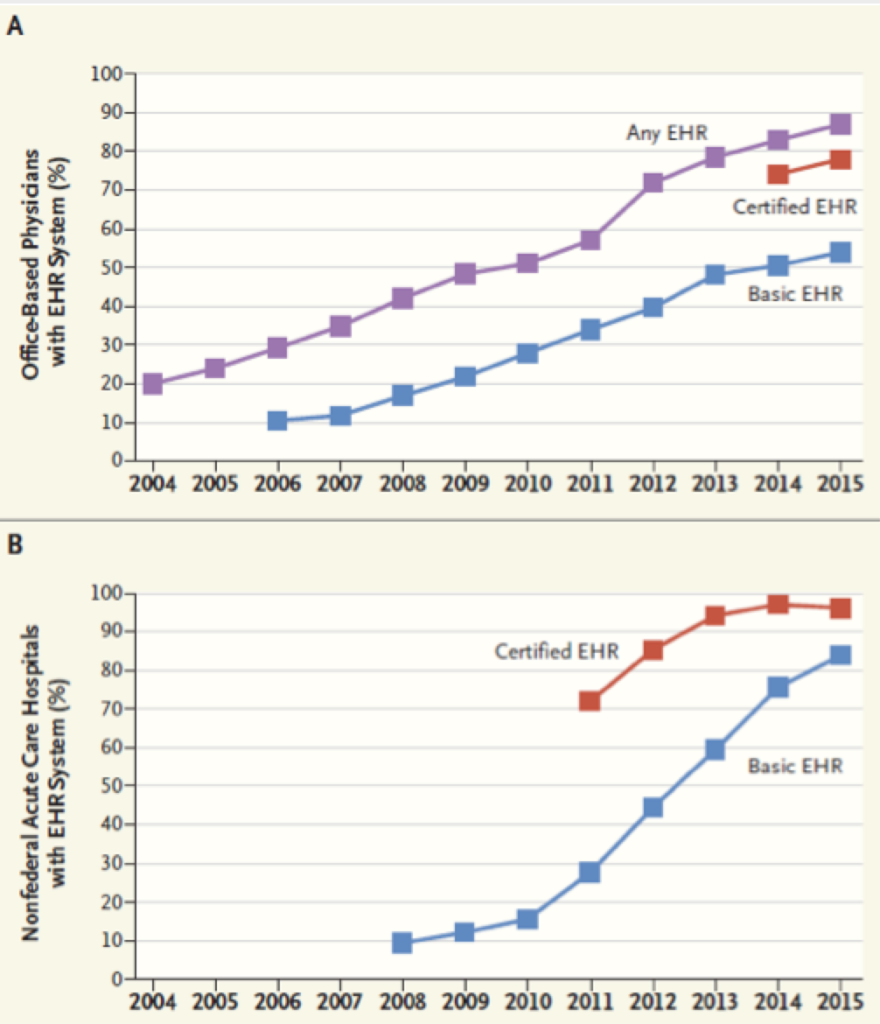
The 4 former National Coordinators rightly point out that the establishment of HITECH is closely correlated with the rapid adoption of certified EHR technology (CEHRT) by both acute care hospitals and physician office-based practices alike. Many of you have seen a reproduction of the graphs proudly displayed in their article which I have reproduced below. Indeed, the carrots and the sticks do appear to have achieved a massive conversion in this country from paper to EHR.
The other side of the coin
The companion piece in the NEJM is written by Drs. John Halamka and Micky Tripathi.2 John, aka the Geek Doctor, is an ER doc and the CIO at Beth Israel Deaconess Medical Center in Boston. For the past decade, John has written a remarkably insightful blog, from which I have frequently found pearls of wisdom. Micky conducted some of the original research upon which the MU framework was based and has been very active in the Health IT space in Massachusetts, as well as Nationally. He is currently CEO of the Massachusetts eHealth Collaborative. I must say, the tenor of their piece is a bit more sobering. They appropriately point out several of the missed opportunities along the way. Not to cherry pick (OK perhaps I’m guilty of a bit of that), but check out these sound bites from their Perspective1:
“Along the way, however, we lost the hearts and minds of clinicians.”
“Burdensome requirements imposed costs on providers and vendors without offering sustained benefits.”
And the coup de grâce:
“It wasn’t just providers who suddenly faced an avalanche of requirements. EHR vendors seeking to innovate had to meet complex certification requirements, administered by ONC-authorized testing companies, that imposed not only direct costs, but large opportunity costs as well. Development resources had to be diverted to programming of complex certification requirements to meet the technical, functional, and workflow requirements of meaningful use, which left little available capacity for innovation and product development based on user experience. Over time, providers and vendors began to perceive meaningful use as yet another check-the-box compliance program.”
Amen, brother—been there, done that!
Both perspectives are worth the read, but if I were to advocate that you read one or the other, my vote would be certainly be the one written by John and Micky.
HITECH and nephrology
So, where did our specialty land with HITECH? In many respects, we made out like bandits, in others not so much. Many nephrologists captured the early MU incentive dollars and some may have even used those dollars to fund the acquisition of CEHRT. As I have noted before, dialysis facilities, like nursing homes, ambulatory surgery centers, and a host of other venues of care, were excluded from the MU framework. This created the unintended consequence of permitting thousands of nephrologists to successfully file for hardship exceptions, avoiding the MU paradox of trying to meet increasingly difficult standards in order to capture a declining financial incentive. In the category of not making out like bandits, is the absence of a clear certification path for dialysis information systems. As Dr. Dugan Maddux noted in last week’s interview with Eddie Hedrick (a man with whom I shared many anxious moments along multiple MU certification gauntlets), information exchange with dialysis clinics (and nursing homes, ASCs, etc.) is even more challenging today than what you face when you try to move patient data from physician office to physician office.
What’s next?
Next steps in this journey will be remarkably important. Whether MACRA and the QPP deliver us to the promised land remains to be seen. Ignoring the price tag, HITECH was a reasonable start and the vast majority of health care providers no longer trap patient information in paper silos. In my view, success in the path ahead involves 2 overarching themes that will require our undivided attention:
- Usability—with a heavy emphasis on User Centered Design
- Interoperability—not interoperability that brings a CCDA into my EHR, but interoperability that is true to the well-worn mantra: the right data for the right patient at the right time.
If during the next 8 years we solve just one of these, I’d ring the bell. Solve both and it’s Nephrology Nirvana!
As fall descends on 2017 and we look forward to 2018, what are your Health IT expectations for the coming years? Drop us a note and join the conversation.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Image from www.canstockphoto.com
1. Washington V, DeSalvo K, Mostashari F, Blumenthal D. “The HITECH Era and the Path Forward.” N Engl J Med 2017;377:904-06.
2. Halamka J, Tripathi M. “The HITECH Era in Retrospect.” N Engl J Med 2017;377:907-09.




Leave a Reply