The Centers for Medicare and Medicaid Services (CMS) recently released a statement announcing that after conducting targeted reviews for the 2017 MIPS performance year, they identified a few errors in the scoring logic that resulted in the underpayment of an unknown number of clinicians.
Whoops!
According to CMS, “the targeted review process worked exactly as intended, as the incoming requests quickly alerted us to these issues and allowed us to take immediate action.”
The biggest culprits that caused calculation errors were the application of the following items:
- 2017 Advancing Care Information (now Promoting Interoperability) extreme- and uncontrollable-circumstances hardship exceptions
- Improvement Activity credit for successful participation in the Improvement Activities Burden Reduction study
- Adding the All-Cause Readmission measure to the MIPS final score
The good news is that CMS has a solution to implement; the bad news is those impacted may not know unless they request a targeted review.
Are we surprised? The MIPS scoring process is so confusing to begin with, it would have been a miracle if CMS had zero issues with scoring calculations in year one.
So, how do you know if your score is wrong? Should you ask for a targeted review?
Know your score
The first step is to see what your score is in the first place. Clinicians or groups should log into the Quality Payment Program (QPP) portal and review their 2017 MIPS performance feedback.
Look to see if any bonus opportunities were not added correctly—or to ensure that you received special status (if applicable).
Although a MIPS score was given to you upon submission, there could have been factors that changed your score as more data became available, such as:
- Scoring updates based on a special status (eg, reweighting the Advancing Care Information performance category to zero percent for hospital-based MIPS eligible clinicians)
- All-Cause Hospital Readmission measure calculations
- CAHPS for MIPS Survey results
- Advancing Care Information hardship exception application status
- Improvement Study participation and results
- Performance benchmarks for Quality measures that didn’t have a historical benchmark (most common for registry-based measures)
Browse through your data and drill down into the different categories of MIPS to see how all the points were assigned. If you feel something is off, then get your evidence ready and request a targeted review.
Scaling factor and budget neutrality
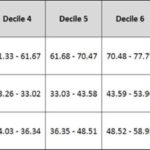
Maybe your score added up correctly, but you’re concerned about the payment adjustment percentage you received.
Each MIPS eligible clinician received a MIPS payment adjustment factor (and an accompanying payment adjustment) based on their MIPS final score.
I can count on 2 hands how many clinicians have approached me shocked about the payment adjustment assigned to them. “I got a 100 out of 100, and I only got a 2% increase? I thought I was going to get a 4% increase.”
If you are an avid Acumen blog reader, you know this isn’t reality.
We blogged about the money in MIPS before, but just to quickly recap—the amount of the positive adjustments is scaled and will depend on the scores as well as the total number of clinicians both above and below the performance threshold. CMS set the bar low in the transition year. As a result, 91% of MIPS eligible clinicians were able to successfully participate.
Also, by law, MIPS must remain budget neutral. CMS may not pay out more in incentive payments than it recoups in penalties. If there are not a lot of losers, there are not a lot of winners.
In summary, don’t request a targeted review just because you didn’t get a 4%. In fact, payment adjustment could actually go down.
Here’s the kicker. As mentioned above, the MIPS program is designed to be budget neutral. Now that CMS has found errors in their scoring, any affected clinicians will most likely receive a higher payment adjustment. If clinicians who are asking for a targeted review end up getting more money, that means others will need to get less.
It is important to keep logging into the QPP portal to see how your percentage may shift!
Still want a targeted review?
At the end of the day, if you feel there was an error in your MIPS score calculation or payment adjustment, you can request a targeted review.
Eligible clinicians, groups, and APM entities can request a targeted review by going to the Quality Payment Program website, logging in using their Enterprise Identity Management (EIDM) credentials, and requesting a targeted review.
If you submitted your MIPS data through a third-party vendor or registry, that entity may be able to request a targeted review on your behalf, but reach out to them to double-check.
Outside of the three main culprits listed above, there could be other reasons to request a targeted review, such as:
- A MIPS-eligible clinician or group has supporting documentation indicating that measures or activities submitted during the submission period and used in the calculation of the MIPS final score and determination of the MIPS payment adjustment have calculation errors or data quality issues. These measures or activities could have been submitted with or without the
assistance of a third-party intermediary - A MIPS-eligible clinician or group has supporting documentation indicating that certain errors were made, such as eligibility being wrongly assigned to the MIPS-eligible clinician or group
- A MIPS-eligible clinician has supporting documentation indicating that they should qualify for automatic reweighting of performance categories due to the 2017 policy for extreme and uncontrollable circumstances
- A MIPS-eligible clinician has supporting documentation indicating that they were erroneously excluded from the APM participation list and should have been scored under the APM scoring standard
However, the targeted review process should not be used to challenge overall program definitions or established methodologies—save that for future proposed rule comments.
Also, you cannot submit a targeted review if you already had one done for that performance year. Targeted review decisions are final and there will be no further reviews allowed.
If you do end up requesting a targeted review, prepare any documentation that will support your claim. CMS may request that you submit supporting documentation within 30 calendar days, including:
- Supporting extracts from the MIPS-eligible clinician’s EHR
- Copies of performance data provided to a third-party intermediary by the clinician or group
- Copies of performance data submitted to CMS
- QPP Service Center ticket numbers
- Signed contracts or agreements between a clinician or group and a third-party intermediary
- APM participation agreements
- Partial QP election forms
Targeted review outcomes will be emailed to the submitter and any specific changes to performance category scores, final scores, and MIPS payment adjustments will be communicated through updated performance feedback.
Due to the calculation slip-up, CMS has extended their due date for targeted review requests. Eligible clinicians now have until Oct. 15, 2018 at 8:00 pm EDT to request a targeted review of their MIPS performance feedback from CMS.
Phew. How’s that for year 1?
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Image from www.canstockphoto.com



Leave a Reply