 I don’t know about you, but the summer doldrums have certainly arrived here in Southside Virginia. Nothing like stepping out into the sauna and having your glasses fog up due to the heat and humidity! There’s no better excuse for staying inside and unpacking the 1,473-page notice of proposed rule-making (NPRM) that defines what may be in store for the Quality Payment Program (QPP) next year. And with the sexy title “Revisions to Payment Policies under the Physician Fee Schedule and Other Revisions to Part B for CY 2019; Medicare Shared Savings Program Requirements; Quality Payment Program; and Medicaid Promoting Interoperability Program,” who could resist?
I don’t know about you, but the summer doldrums have certainly arrived here in Southside Virginia. Nothing like stepping out into the sauna and having your glasses fog up due to the heat and humidity! There’s no better excuse for staying inside and unpacking the 1,473-page notice of proposed rule-making (NPRM) that defines what may be in store for the Quality Payment Program (QPP) next year. And with the sexy title “Revisions to Payment Policies under the Physician Fee Schedule and Other Revisions to Part B for CY 2019; Medicare Shared Savings Program Requirements; Quality Payment Program; and Medicaid Promoting Interoperability Program,” who could resist?
This beast was released on July 12, along with this handy 28-page summary. This year the QPP content was combined with the annual physician fee schedule NPRM, leading not only to an awkward title, but a tome chock full of intrigue. Can you believe they are actually considering consolidating the common office-based family of E&M codes that you use every day into single codes with a single payment rate? Bet they hear a lot about that from organized medicine! Today we are going to steer clear of that madness and focus on some of the juicy QPP tidbits, but rest assured this will not be the last Acumen blog post related to this proposal.
First, let me say that I have been reading these things for many years and I have come across my fair share of flowery language. I have to tell you, however, this NPRM is full of lingo that suggests they are truly trying to lighten the proverbial load and make life a little easier for providers. Phrases like “Patients Over Paper” and “Meaningful Measures” course throughout this rule. They almost have me convinced…almost.
Category weighting
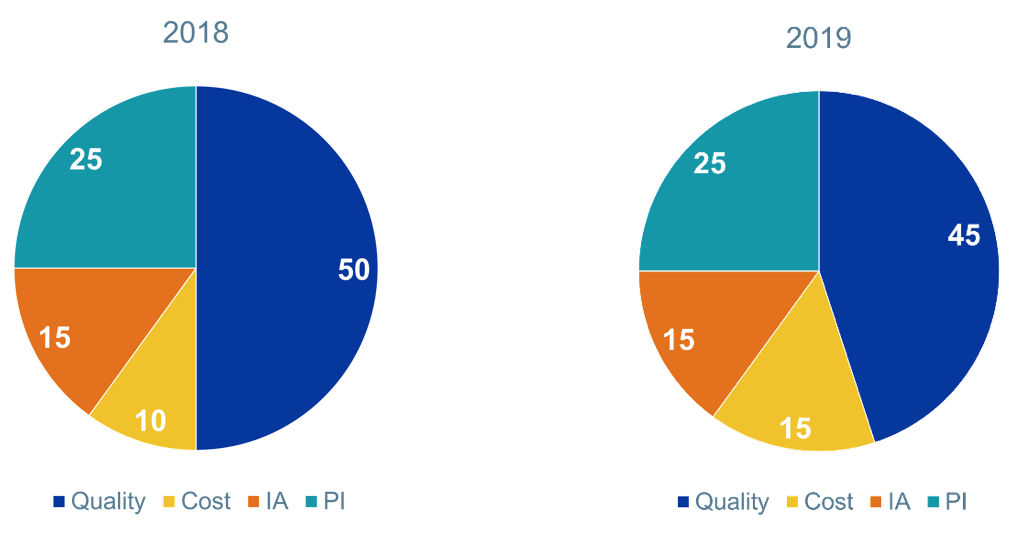
Let’s start with the easy stuff. As you may recall, MIPS is made up of 4 categories; Quality, Resource Use (Cost), Improvement Activities, and Promoting Interoperability, which used to be called Advancing Care Information, which used to be called Meaningful Use. (Really, you can’t make this stuff up.) Take a look at the graphic below, which shows the current mix (i.e., what we will see next year if the NPRM comes to fruition).
MIPS Category Weightings
The big news here is this: Cost was originally supposed to ramp to 30% of the MIPS score in 2019, putting it on equal footing with Quality, which was due to drop to 30%. But based on feedback the folks at HHS have received, they intend to slow walk the rise of the Cost component. In fact, they propose to bump this category’s weight by 5% per year such that they will reach the 30/30 mix referenced above in time for payment year 2024.
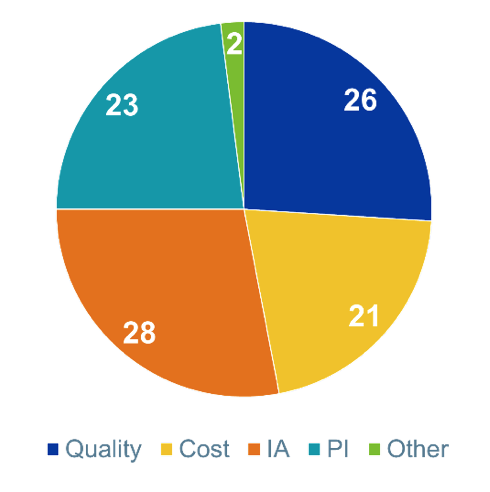
While we are talking category weights, I cannot help but reference an article I read last week in Health Affairs.1 The authors claim to have conducted the first physician survey since MIPS launched in 2017. Among the many things they asked the docs who participated was, How would you weight the MIPS categories? Their response? Check out the pie chart below.
Survey Respondents
These docs clearly favor Improvement Activities and they are not afraid of the Cost category. The article is worth a look if you get a chance.
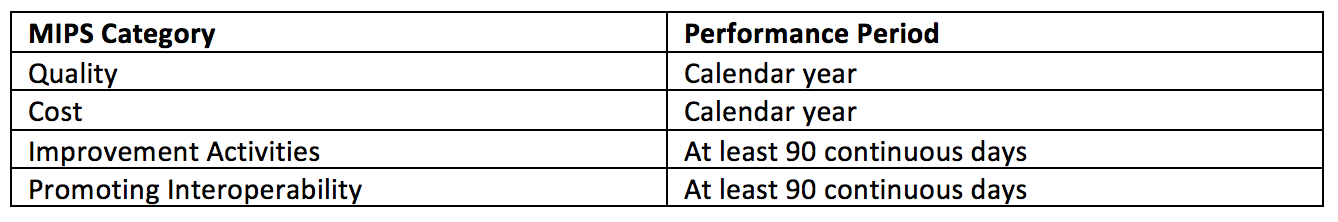
Performance period
Nothing fancy here other than the proposal to lock in the performance periods for everything but Promoting Interoperability. The table below highlights each MIPS category’s performance period. They are proposing these performance periods for all future years, with the exception of PI, for which they slyly limit the proposed extension through payment year 2022.
Quality
A few high-level changes of interest here, and a lot of devil in the detail, which we will likely address in future posts. They are making a concerted effort to move away from process measures and towards outcomes measures. They also intend to abandon claims-based reporting, but will make an exception for small practices. In addition, there is a distinct interest in adding patient-reported outcome measures, affectionately referred to as PROM. In this setting they are retiring 34 existing quality measures, adding 4 PROMs, 7 high-priority measures, and “2 other measures on important clinical topics in the Meaningful Measures framework.” There’s that phrase again! Of interest to nephrology, 3 of the measures in the existing nephrology set are being removed:
- Screening for future fall risk (although this is being replaced by the fall-risk measure, which looks remarkably similar to the one in use today by the ESCO program)
- Adult Kidney Disease: BP management
- Pediatric Kidney Disease: Adequacy of volume management
Changes to the measures aside, what I find most intriguing about the Quality category is buried deep within this NPRM. As you may be aware, reporting quality for MIPS as a hospital-based doc was a bit of a nightmare. In the interest of reducing administrative overhead, they have moved to what’s referred to as “facility-based measurement.” So, if you are a doc like a hospitalist, you may wish you could lean on the quality measures the hospitals already report instead of harvesting your own quality data and figuring out how to get it to CMS. Well, in this NPRM they are asking for comment about 2 additional facility-based venues of care. One is post-acute (think SNF, LTAC, etc.). The other? Wait for it, wait for it…yep, the dialysis clinic.
The NPRM correctly points out that the ESRD QIP was the first value-based payment program in which a provider’s payment was tied to performance. What they don’t say is the QIP is basically a claw-back program, a means to penalize “poor performance” without offering the potential for upside. Nevertheless, they are asking for comments about the possibility of allowing nephrologists to use dialysis facility QIP scores, modified in a fashion that works for MIPS, as an alternative to the current approach (picking from the laundry list of MIPS quality measures and selecting a method to get those MIPS measures to CMS). This would certainly reduce administrative overhead for docs, and I must admit, it’s an intriguing thought. But I see a very heavy lift here. And given the changes recently proposed for QIP, well, let’s just say I don’t anticipate the line of nephrologists waiting to report QIP measures will be very long.
Cost
The last topic on my category list today is cost. The big news about the Cost category is the slow walk I mentioned above, where 2019 sees this category rise from 10% to 15%. Of interest, those tricky episode-of-care metrics are indeed raising their head in 2019. There will be 8 of these guys introduced in 2019 within the MIPS Cost category. As I review the list of 8, I do not see one that nephrologists are likely to be tagged with. I think this is wonderful news as it allows us to watch how others fair with this new addition to the Cost category before we are exposed as a specialty. My sense is that we will not have to wait long. This category deserves more attention in the future, but I am going to wait for the final rule.
Odds and ends
A couple of other things are worth a quick mention. They have tweaked the low volume threshold (LVT) in a very odd way. On the surface this looked bizarre; taking a deeper dive only confirms that notion. They have added a 3rd LVT category—not so more docs can escape MIPS, but so more docs who are excluded by the LVT can “opt in” to MIPS. Really, that’s not a typo. No impact for us, but very strange indeed.
They have also expanded the pool of provider types now exposed to MIPS. Joining the growing list of MIPS eligible clinicians in 2019 will be physical therapists, occupational therapists, clinical social workers, and clinical psychologists. I point this out, not because it directly impacts nephrology, but I think it’s a signal that MIPS is here to stay in spite of MedPAC’s expressed desire to replace it.
More to come
1,473 pages is a lot to cover in a blog post, even in the sweltering heat of mid-July. However, this is where our journey ends today. All of you know my colleague Diana Strubler, and rest assured she is on deck and will fill in the gaps, perhaps reviewing Improvement Activities and (teaser alert) letting you know about the exciting changes this NPRM holds for the category formerly known as Advancing Care Information Meaningful Use. I am certain that in future posts you will find additional detail harvested from this NPRM. Until then, stay hydrated and remember that famous renal-related saying, “clear and copious.”
Do you have a comment about the 2019 NPRM? If so ship it to HHS before September 10, or better yet, drop us a comment here at the Acumen blog and join the conversation. It’s easy to do and beats stepping out into the dog days of summer!
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Image from www.canstockphoto.com




Mohammed Alzubaidi says
The 2019 NPRM “one size fits all” proposal has many pitfalls:
1. With regards to nephrology, patients we see in renal clinic tend have complicated medical conditions and are sicker. I worry that notes will becomes electronic version.
2. it takes a lot more time to see a patient with complex issues. It could easily lead to cherry picking (docs avoiding sicker patients, more challenging patients, lower income patients).
3. Documentation when “proper” shows intellectual effort, is educative, and is a safe way of communition between provides.
Mohammed Alzubaidi says
Correction:
1. With regards to nephrology Patients we see in renal clinic tend have complicated medical conditions and are sicker. I worry that notes will becomes electronic version OF TOILET PAPER.