Last week, I received a call from a nephrologist who works at a small practice. Let’s just call him Dr. Smith for anonymity. The call went something like this…
Dr. Smith: “Diana, I am looking at my MIPS dashboard and I think I’m doing well. What do you think?”
Diana: “It looks like you are doing great at Advancing Care Information. You are scoring around 105 points and you only need 100!”
Dr. Smith: “I chose our practice’s improvement activities. I’m sure we will get the full points here…”
Diana: “Great! Make sure you document how you are meeting each activity. The last area to look at is quality. This is the trickiest one of them all!”
Dr. Smith: “I don’t get it. I am getting a 90% in most of my measures…isn’t that good?”
Diana: “That does sound good. However, when compared against the national benchmarks for most of these measures, a 90% may only earn you around 5 (out of 10) points per measure. The quality category is worth 60 points (each of the 6 measures will be worth 10 points each). If you only get around 5 points for each measure, you will only score a 30 out of 60 in this category.”
Dr. Smith: ***lots of unmentionable comments and noises*** “You are kidding! This program is impossible for nephrologists!”
Wow, that call escalated, didn’t it? Let’s take a deeper look into what happened here because I’m afraid this will be an all-too-common scenario!
Understanding measure selection, measure submission, and the case of the “topped out” measure are very important when assembling your Merit-Based Incentive Payment System (MIPS) quality strategy.
Quality measure selection
Choosing your 6 quality measures is something you will want to do early on. It’s hard to do well when you don’t know what to do! If it were me, I’d choose more than 6 (just so I had some back up options).
When selecting quality measures, you will want to keep the following in mind:
- Is it applicable to my scope of practice?
- Will I have at least 20 patients that meet the denominator?
- Can I report this measure on over half of the patients that meet the population criteria?
- How well did I do on this measure in the past (if applicable)?
- Does this measure qualify for any bonus points (is it a high priority or outcomes measure)?
- What are the established benchmarks for this measure? (More on this below.)
- Is this measure topped out?
- What if there are no benchmarks?
- What data submission method will I use?
- Some measures can only be reported using one submission method such as a QCDR/registry.
- All 6 measures must be reported via the same data submission method.
The QPP website provides a list of 271 measures that you can choose from. This list does not include certain measures that may only be reported via a Qualified Clinical Data Registry (QCDR).
Quality benchmarks
I’ve written about quality benchmarks here before. In a nutshell, prior to every performance period, CMS will post the benchmarks for all MIPS quality measures (utilizing a baseline performance expectation that reflects 2 years before the current performance period).
These benchmarks will let CMS know how you stack up against everyone else in the country. Remember, you are competing against everyone else who reports that measure (and you are not given special treatment just because you are a specialist).
Looking at the benchmarks for every measure is a very important thing to do. Without knowing the benchmarks, you will not know what your goal performance score should be.
Also, keep in mind that the same measure may have up to 3 different benchmarks, depending on the data submission method selected.
For example, the “pneumonia vaccination status” can be reported via 3 different submission methods. If you received an 86% performance score, you could fall into 3 different deciles.
You would be in decile 8 (if reporting via claims), decile 9 (if reporting via registry/qcdr), and decile 10 (if reporting via EHR).
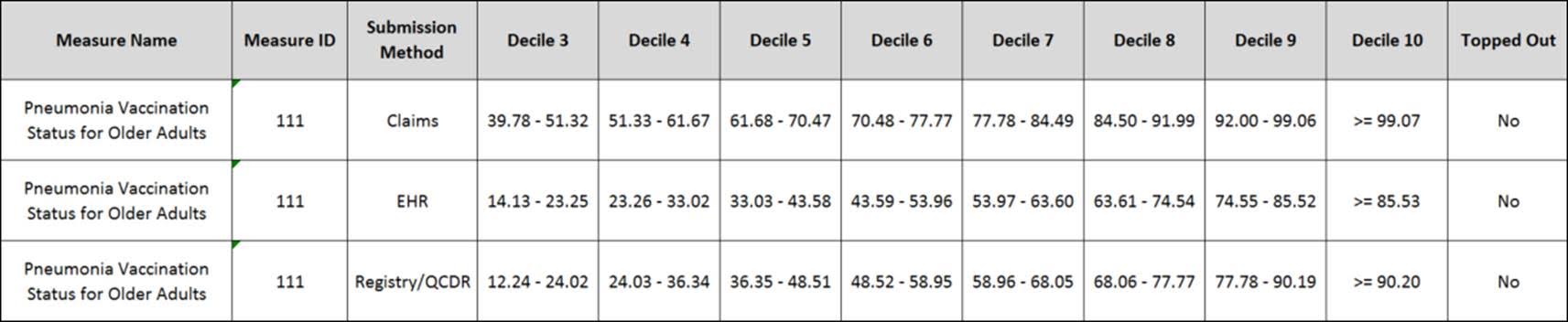 In this case, reporting via EHR would be more favorable.
In this case, reporting via EHR would be more favorable.
Lastly, be aware when choosing measures without benchmarks.
If you find a measure you really like, but it’s a new measure (meaning it is newer than 2 years old and does not have a benchmark), CMS will attempt to calculate a benchmark based on the current year’s performance data. That means you will have no idea how well you did until after your data is submitted. If a benchmark couldn’t be established, you will only get 3 points! More on that here!
Topped out
Choosing “easy” measures may not be a great strategy. CMS considers certain quality measures to be “topped out” or no longer meaningful. A “topped out” measure is one where overall performance on that measure is very high and there is little room for improvement. Oftentimes these measures are on the short road to retirement.
A great example of a “topped out” measure is “documentation of current medications.” If you choose to report this measure via claims or a registry, you would have to get a perfect 100% to land in decile 10. Otherwise a 99.99% would get you in either decile 5 or decile 7!
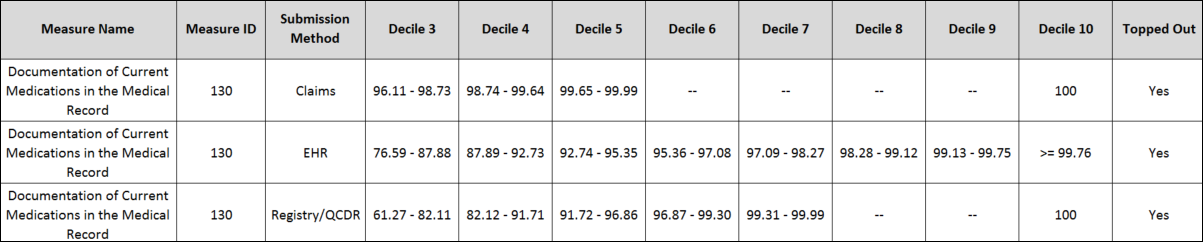 To complicate things a little more – a measure can be topped out in one reporting mechanism but not another. For example, the tobacco screening measure is considered topped out when reported via claims but not when reported via EHR or QCDR.
To complicate things a little more – a measure can be topped out in one reporting mechanism but not another. For example, the tobacco screening measure is considered topped out when reported via claims but not when reported via EHR or QCDR.
A majority of the “topped out” measures can be found in both the claims and registry/QCDR submission methods. Topped out measures make up 70% of all measures offered via claims and nearly 50% of MIPS measures offered via registry/QCDRs.
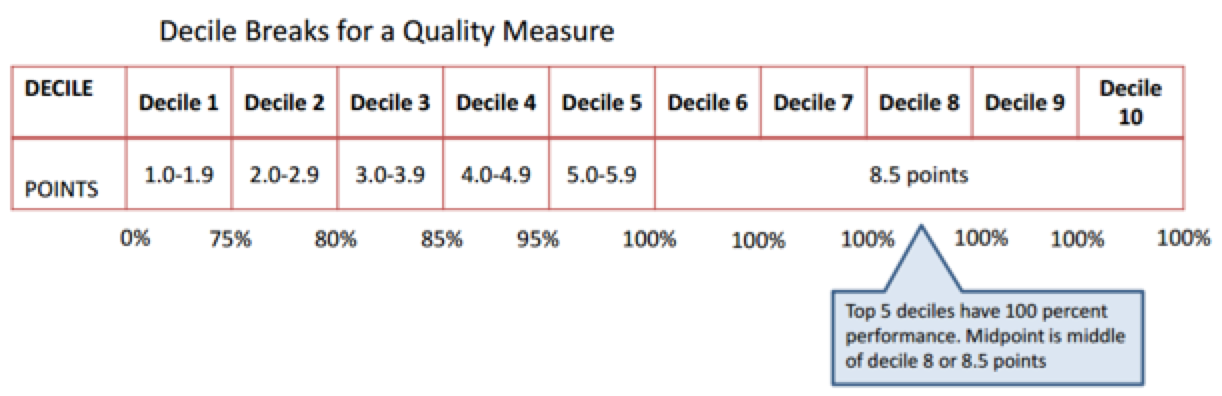
In future years, CMS may consider a different scoring approach for “topped out” measures. For example, they threw around the idea of a “mid-cluster scoring” approach. This means that if half of all eligible clinicians are reporting a particular measure with a score of 100%, then the middle of that decile cluster is the value that the performance rate will be assigned.
For example, in the figure below, the middle of the cluster is in the middle decile 8 (or 8.5 points). All clinicians with a 100% performance in this measure will only earn 8.5 points.
Choosing a “topped out” measure won’t hurt you initially, but down the road, when the MIPS composite performance score threshold gets higher, you may want to find measures where the difference between a 99.99% and a 100% are not 5 deciles apart.
A little relief
Since the measure benchmark scoring concept is new, CMS finalized a measure score “floor” of three points for the 2017 performance year. That means if you just submit “something” for one measure you will earn no less than 3 points (which is enough to avoid a MIPS penalty in 2019).
This year is also a transition year, meaning you don’t need to submit any quality data (as long as you submit data for one of the other MIPS categories). If you go this route, make sure you still keep an eye on your quality scores and come up with a plan for next year.
If one transition year isn’t enough for you, rumor has it that the MACRA 2018 final rule (which will most likely drop in the coming weeks) may provide additional reprieve. The new Health and Human Services Secretary Tom Price is expected to extend flexibility in 2018 as well.
Or you could always try your luck to see if you’re excluded from MIPS. The Quality Payment Program (QPP) website recently launched an eligibility checker that will let you know if you are in or out for 2017. Dr. Ketchersid and Dr. Maddux – don’t worry, I checked for you both and you’re excluded!
What are you doing to prepare for the quality component in MIPS? What measures are you selecting? We would love to hear your plans below!
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.





Leave a Reply