 Happy New Year Acumen blog readers! I hope 2019 is off to a wonderful start for each of you. Dr. Maddux finished last year off with a remarkable post. If you missed it, I’d suggest taking a look here. That parachute post is a tough act to follow, but I am going to give it the old college try and wow you with a riveting post about, wait for it, wait for it…the Quality category within MIPS! Can’t wait, right?
Happy New Year Acumen blog readers! I hope 2019 is off to a wonderful start for each of you. Dr. Maddux finished last year off with a remarkable post. If you missed it, I’d suggest taking a look here. That parachute post is a tough act to follow, but I am going to give it the old college try and wow you with a riveting post about, wait for it, wait for it…the Quality category within MIPS! Can’t wait, right?
The basics
As noted recently in a post by Diana, the Quality category represents 45% of your score this year, down from 50% last year. At 45%, Quality remains the most important contributor to your overall MIPS score in 2019, which as we know will have a direct impact on your 2021 Medicare Physician Fee schedule. The Quality category for 2019 looks a lot like it did last year, so I would highly recommend rereading Diana’s excellent post from 2017. With rare exception, you still must report on at least 6 quality measures, including at least 1 outcome measure, and this year there are over 250 measures to choose from. The performance period for Quality remains the entire calendar year. That’s right, the Quality clock for 2019 has been ticking for almost a full week now! As a supplement to this post, you may want to peruse this handy fact sheet produced by our good friends at the agency.
One final note regarding the basics of the Quality category, last year’s small practice bonus was 5 points added to the total MIPS score for providers in practices with 15 or fewer NPIs. This year they have moved the small practice bonus to the Quality score. You will receive 6 Quality points instead of 5 MIPS points if you are in a small practice, which in effect lessens the benefit compared to last year. Most of the other Quality-related bonuses remain intact for 2019.
Specialty measures
As in years past, CMS attempts to make life easy for specialists by publishing “specialty sets,” which are collections of measures they believe appropriate for specific specialties to report. Of interest, there is a nephrology specialty set (Table B.19 in the appendix of the final rule). The nephrology specialty set includes 15 measures this year, and yes, a few of these do indeed look like measures a nephrologist might report. Note if you go down this path, the 6 you choose most all come from this list of 15. To make a life a little easier, you can locate the nephrology measure set on page 2245 of the PDF located here.
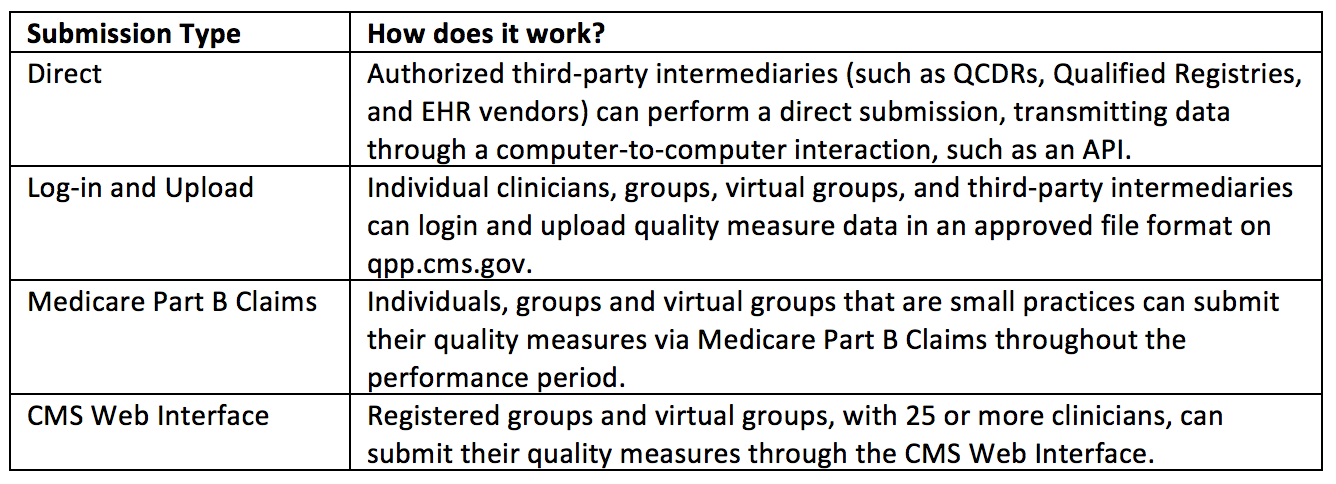
Submission methods
Thankfully, submitting data to CMS essentially remains the same for 2019. CMS has attempted to clean up some of the confusing lingo related to data submission. I will let you be the judge of whether or not they have succeeded. Below are some details repurposed from this reference:
And one final point about data submission, unlike in years past, you can now mix and match data submission types for Quality and receive credit for each of your submissions.
Benchmarks are important
As you make your way through the morass of selecting at least 6 Quality measures to report, make sure to consider each measures benchmark. For most, but not all the available Quality measures, CMS publishes benchmarks based on historic data. Importantly, the benchmark for the same measure can, and in many cases does, vary based on the submission method. Here’s a classic example for the measure Diabetes: Hemoglobin A1c (HbA1c) Poor Control (>9%). And yes, surprisingly this is one of the 15 measures in the nephrology measure set.
2019 Benchmarks for Measure 001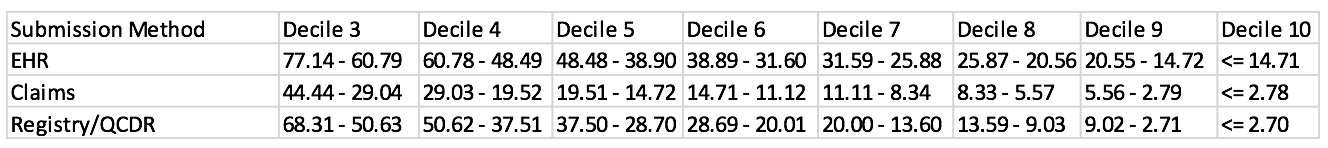
What in the world does this table mean? Well, assuming you have at least 20 patients that meet the measure’s eligibility, and you meet the data completeness standard (which typically means you report on at least 60% of your eligible patients), then in order to achieve the maximum number of Quality points for this measure when reporting via your EHR, ≤ 14.71% of your reported eligible patients have a HbA1c > 9%. But, if you submit this measure through a registry or a QCDR, maxing out on this Quality measure is tougher as you only receive the maximum number of points if ≤ 2.7% of your eligible reported patients meet the target. Clear as mud? The easiest way to locate the benchmarks for 2019 is to scroll down to page 16 of this PDF and click the Quality benchmark link. Take a look before you select your measures…you will happy you did.
Topped-out measures
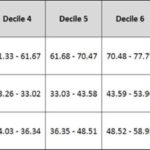
While the concept of benchmarks is fresh on your mind, make sure you think twice about signing up to report a “topped out” measure. Check out the table below, which includes the 2019 benchmarks for Documentation of Current Medications in the Medical Record (yep, another member of the nephrology measure set):
2019 Benchmarks for Measure 130
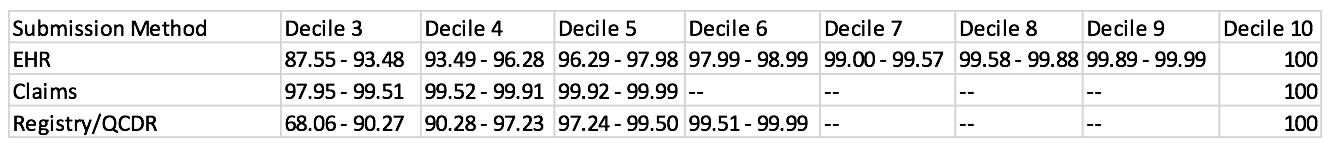
Now you might be thinking, how hard can this be? We always document the med list when the patient comes into the office. Well, if you pick this measure you better hope you don’t miss a single patient. To achieve a perfect score for this topped-out measure, 100% of your reported patient encounters must have the med list documented. Miss a single encounter while reporting through claims or a registry and you fall off a cliff, dropping to the 5th or 6th decile respectively!
While we are on the subject, the final rule has now made it clear that “extremely topped out measures” (think average scores across the country in the 98th-100th percentile) will be quickly retired from the program. And speaking of retiring measures, this final rule makes it very clear that process measures are in the crosshairs as well. Increasingly the measures available are likely to be a combination of outcome measures, high-priority process measures, and patient-reported outcomes. Finally, they truly want to eliminate claims-based reporting, but with a nod to small practices, for 2019 they will continue to accept this data-submission method if you are in a practice with 15 or fewer providers.
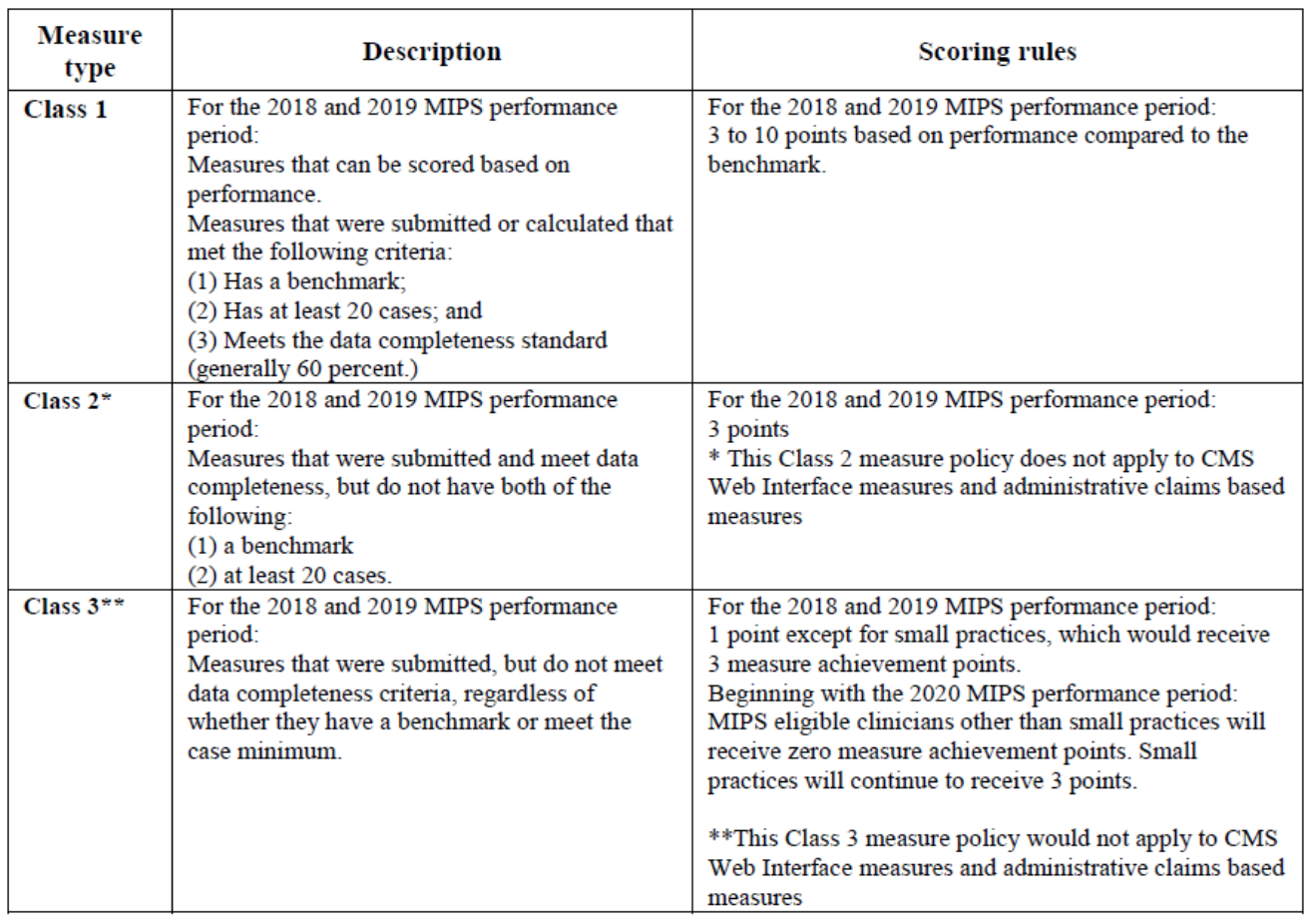
20 case minimums and data completeness
Your measures’ benchmarks are not the only thing you should consider. You need at least 20 cases to be eligible for maximum Quality points for the measures you report, AND you need to clear a data completeness hurdle. In most instances you will meet the data completeness standard by reporting on at least 60% of the patients you encounter who meet the measures inclusion criteria. The table below from the final rule highlights the combined importance of the presence of a benchmark, having at least 20 cases, and meeting the data completeness standard:
Scoring Rules for Quality Measures in MIPS
Year-over-year improvement
Last but not least is the opportunity to capture Quality points based on year-over-year improvement returns for 2019. You are eligible for improvement points if you reported quality in 2018 and do so again in 2019. At a high level, the way this works is as follows: strip out the bonus points from both years and compare your overall score in 2019 with your score in 2018. If you achieve a higher percentage of the available Quality points in 2019 when compared with 2018, you will collect improvement points. The math here is pretty simply and there’s a nice example on pages 20-21 of this PDF.
Next steps
I know what you are thinking, participating in the parachute study Dr. Maddux reviewed for us last week would have been easier than reading this MIPS Quality post! To simplify the complex, I think this comes down to a few choices:
- Report Quality as a group or as an individual (most are likely to choose to report as a practice, which is the group path)
- Determine your submission method of choice now (don’t wait until December)
- Select your Quality measures (I’d start with more than 6 and check your progress throughout the course of the year)
- As you select those measures, keep 3 things in mind:
- Can we meet the data completeness standard (typically 60%)?
- Will we see at least 20 cases?
- What’s the benchmark?
After that, it’s as simple as pulling the rip cord! Happy New Year all. Everyone at the Acumen blog wishes you a safe and prosperous 2019.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Image from www.canstockphoto.com



Ricky Ben says
The aim of the MIPS quality program is to encourage physicians to offer value-based healthcare services to patients. So, they get incentives and bonuses as a reward for their services. It will only be possible when the quality of services will improve. If you look closely into MIPS performance categories, it is obvious that they all add value to the quality of healthcare. Hence, MIPS holds no compromise on quality, and it is indeed the only success formula.