 The plan for this blog post was going to be a continuation of what Dr. Ketchersid so effortlessly delivered last week—a peaceful stroll through the remaining highlights of the 2019 QPP Proposed Rule.
The plan for this blog post was going to be a continuation of what Dr. Ketchersid so effortlessly delivered last week—a peaceful stroll through the remaining highlights of the 2019 QPP Proposed Rule.
However, those wishes came to a screeching halt after I began digging through all 1,472 pages. I was literally gasping as if I were reading a thrilling novel. All the twists and turns had me at the edge of my seat!
In all reality, I was floored by the substantial changes that were proposed, specifically in the category of Promoting Interoperability (PI). There were so many proposed changes to PI that they might as well throw in another name change.
Here’s hoping you stayed hydrated from last week’s post, because things are about to get even hotter.
A higher performance threshold
Before I hop into my favorite category of PI, let’s talk about the magic number. The number you must be at or over to avoid a penalty—the MIPS performance threshold.
In the first year of MIPS, the performance threshold was set to 3 points. It was pretty much impossible to get below 3 points (unless you didn’t participate at all). In the current year of MIPS, the performance threshold is set at 15 points, which is still a relatively low bar.
For the third year of MIPS, CMS is proposing another slight increase by setting the performance threshold at 30 points and the exceptional performance threshold at 80 points (up from 70). The average clinician score in 2017 was in the 60s, so 30 should be easily achievable.
As required by statute, those receiving a score of under 30 points can receive up to a maximum negative payment adjustment of -7 percent. Positive payment adjustments can be up to +7% (but they are multiplied by a scaling factor to achieve budget neutrality). Keep in mind, the maximum positive adjustment is highly unlikely.
MIPS clinicians who had a perfect MIPS score in 2017 will only see around a +2% increase in the 2019 payment year. CMS predicts that eligible clinicians with a perfect MIPS score in 2019 may receive around a +5.7% increase in 2021. This figure can change very quickly based on several moving parts that must be finalized (# of participants, # of participants that receive a penalty, the ease of earning points under MIPS categories, etc). In other words, don’t assume you will get the maximum positive adjustment.
A smaller set of PI measures
Now, on to the star of the show. Of all the categories under MIPS, PI was hit the hardest. As someone who works with software developers, trainers, support staff, and customers, it is always a scare to see such dramatic changes in this category (good or bad). Every change requires a lot of time and money to reconfigure, relearn, and undo.
CMS decided to only focus on measures that support greater electronic health record interoperability and patient access.
As a result, the following list of measures are proposed to be cut:
- Request/Accept summary of care
- Clinical Information reconciliation
- Patient-generated health data
- View, download, or transmit
- Patient-specific education
- Secure messaging
The following measures are proposed to be retained (but with modifications):
- Send a summary of care (name change to “support electronic referral loops by sending health information”)
- Provide patient access (name change to “provide patients electronic access to their health information”)
- Immunization registry reporting (added exclusion opportunities)
- Syndromic surveillance reporting (added exclusion opportunities)
- Electronic case reporting (added exclusion opportunities)
- Public health reporting (added exclusion opportunities)
- Clinical data registry reporting (added exclusion opportunities)
The following measures are proposed to be added:
- Query of Prescription Drug Monitoring Program (PDMP) – optional in 2019
- Verify Opioid Treatment Agreement – optional in 2019
- Support Electronic Referral Loops (a newer version of “request/accept summary of care”)
As you can see, they cut all measures that didn’t directly relate to interoperability and patient’s access to their electronic health information. CMS has also committed to combatting the opioid epidemic by adding measures that support HHS’ 5-point opioid strategy. CMS hopes that the 2 optional e-prescribing measures above will become required beginning in 2020 and beyond.
From optional to required
Unlike this year and last, the proposed rule takes away the ability for eligible clinicians to choose their performance measures. Instead, eligible clinicians will be required to report on all 6 measures from 4 categories below.
The only flexibility given is choosing two public health/clinical data measures and reporting on the 2 optional/bonus e-prescribing measures.
The requirement of the public health/clinical data measures will be the most difficult in my opinion. Now that 2 must be selected, clinicians will have to understand how to collect the required data and implement new interface feeds and any additional costs associated.
Most of the measures above have exclusions. Unfortunately, I doubt most nephrologists will qualify.
Some may be quick to recognize that security risk analysis isn’t listed above, but it is still required as part of your annual attestation (just not scored like it was last year).
Harder to score
Due to the shorter lineup, CMS is also proposing the removal of the “base score + performance score + bonus score” format that is currently in place. This to me is HUGE.
The current PI scoring format is fairly easy to do well in. By just performing the base score you already get 50 out of the 100 points in this category.
In the new proposed setup, you earn points solely based off your performance in the required measures.
My estimate (if this is finalized) is most clinicians will see their PI score drop by quite a bit. There are no more “easy” points given by just reporting the base score on 1 patient.
Let’s walk through an example:
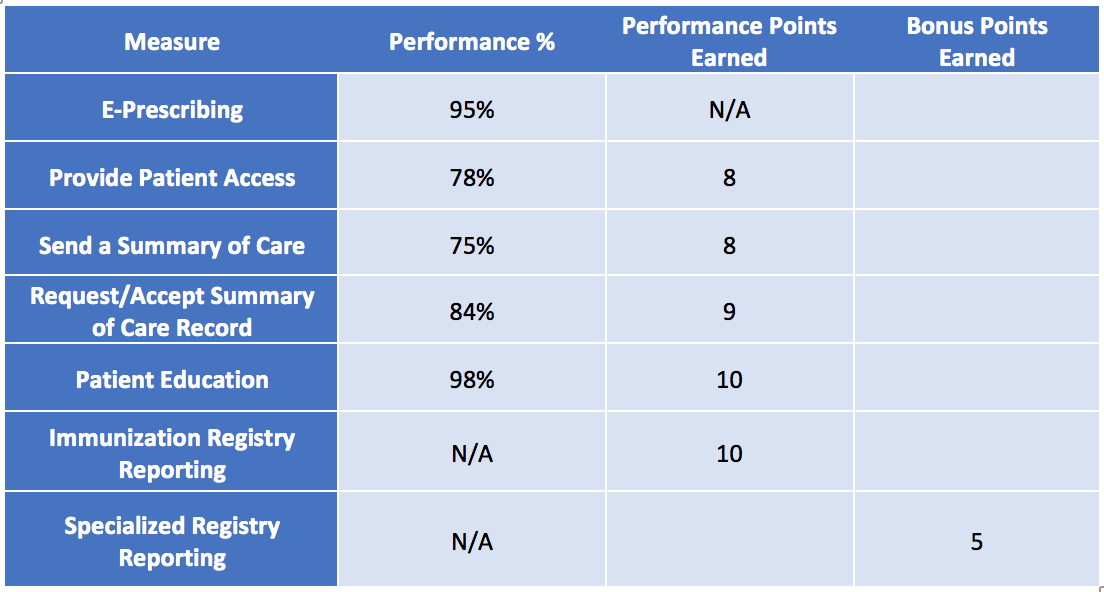
In 2018, Dr. Jones met her base score. She got 50 points. She also earned performance points by reporting the following measures:
The total number of performance and bonus points gave her another 50 points. This gives her a perfect overall PI score at 100/100 points! This will give her the full 25% PI category points under MIPS.
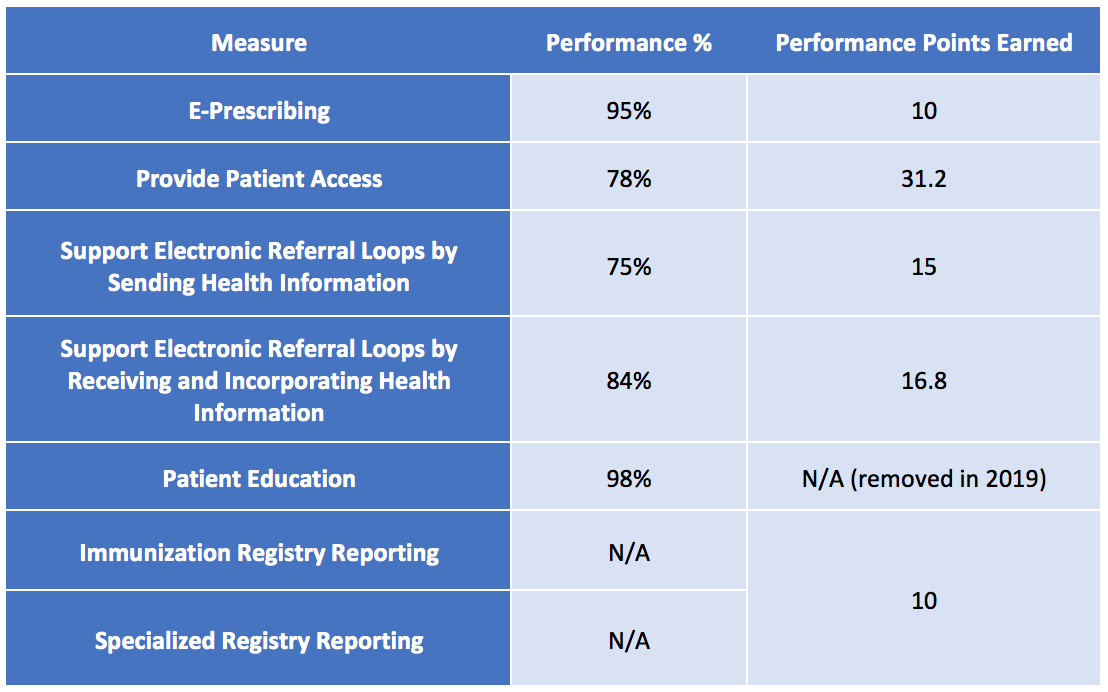
Now, let’s calculate the same performance using the proposed 2019 calculations and let’s assume Dr. Jones kept the same workflows as 2018.
Under the new lineup, Dr. Jones will now only receive 84/100 PI points. This results in 21/25 category points under PI (a 16% drop in performance).
Hopefully this illustration shows why it would be harder to get a better score. My example also made Dr. Jones look great on the interoperability front—in reality, those interoperability measures are very difficult (another topic for another day).
Before you panic, remember that everything above is proposed and not set in stone. However, keep your eyes wide open during the ride.
In an effort to spare our lovely editor, and not turn our blog into a dissertation, I will stop here. However, we’ve only scratched the surface! We haven’t covered improvement activities, physician compare 5-star ratings, or the major changes in bonus points.
There is so much more to unpack in this proposed rule that we will save for future blog posts so stay tuned. In the meantime, we would love to hear your opinions on the proposed PI category. Share your thoughts below!
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Image from www.canstockphoto.com






Leave a Reply