 November is here and before long we will be welcoming the New Year. Following a remarkably exciting World Series, I am delighted the college hoops season is underway. The usual suspects are at the top of the preseason rankings, and I could not help but notice the top two teams square off tomorrow night! Alas, a sports update is not what brought you to the Acumen blog today. It’s our new “friend” the Medicare Quality Payment Program (QPP) which now has your attention. With little fanfare the 1,653-page tome known as the 2018 QPP final rule was set free on November 1. And although the lure of college hoops is tough to ignore, let’s peel back a few layers and see what the QPP has in store for 2018.
November is here and before long we will be welcoming the New Year. Following a remarkably exciting World Series, I am delighted the college hoops season is underway. The usual suspects are at the top of the preseason rankings, and I could not help but notice the top two teams square off tomorrow night! Alas, a sports update is not what brought you to the Acumen blog today. It’s our new “friend” the Medicare Quality Payment Program (QPP) which now has your attention. With little fanfare the 1,653-page tome known as the 2018 QPP final rule was set free on November 1. And although the lure of college hoops is tough to ignore, let’s peel back a few layers and see what the QPP has in store for 2018.
Complexity
One of the reasons this beast requires thousands of pages to explain is that it’s complex. There are literally dozens of nuances, most aimed at making the QPP “easier” for eligible clinicians. The more I read it, the more it reminds me of the multitude of “loop holes” in the federal tax code. While reading the entire rule might become the latest cure for insomnia, thankfully there are a couple of useful PDFs that provide us with a taste of what’s to come. The first is a high-level fact sheet. It is well written and worth a look, but I almost fell out of my chair laughing when I came across this quote in the first paragraph:
As we go into the second year, referred to as “The Quality Payment Program Year 2,” we have been listening to feedback and using it to ensure that:
- The program’s measures and activities are meaningful
- Clinician burden is minimized
- Care coordination is better
- Clinicians have a clear way to participate in Advanced APMs
1,600-plus pages to minimize our burden and make our lives easier? Really? At least there’s a 21-page executive summary that’s truly worth a read. Let’s take a closer look at what they’ve done.
Low-volume threshold
As suggested in the proposed rule, the low-volume threshold exclusion rises to 200 patients or $90,000 of Part B spend in 2018. If you are an eligible clinician that encounters fewer than 200 Medicare beneficiaries during the year OR your annual Part B claims fall short of $90k, you are excluded from MIPS. This one is worth your attention if you employ advanced practitioners. But as I have said before, I think this is bad news for nephrologists. Remember MIPS is a budget-neutral program, a zero-sum game in which participants compete with each other across the breadth of medicine. Very few nephrologists will be exempt due to low volume, and those in MIPS will now face a more competitive pool of MIPS providers, one that’s likely dominated by very large practices.
Cost is back
As you may recall, MIPS has four categories. Among those four, cost is not scored in 2017 and the proposed rule suggested that would be the case in 2018. But cost has raised its ugly head in the final rule and in 2018 the cost category will make up 10% of your final MIPS score, moving to 30% in 2019. Per the final rule, CMS will score the Medicare Spending per Beneficiary and the total per capita cost measure in 2018. These are two of the original cost components within the recently retired Physician Value-Based Payment Modifier. Thankfully they are NOT going to score the episode-based measures they originally planned to count in the cost score. As a reminder, there are no data reporting requirements for the cost category of MIPS. This information is harvested by CMS from administrative claims data. For those keeping score at home, this is how the relative weights shake out in the years ahead:
MIPS Category Weightings by Year
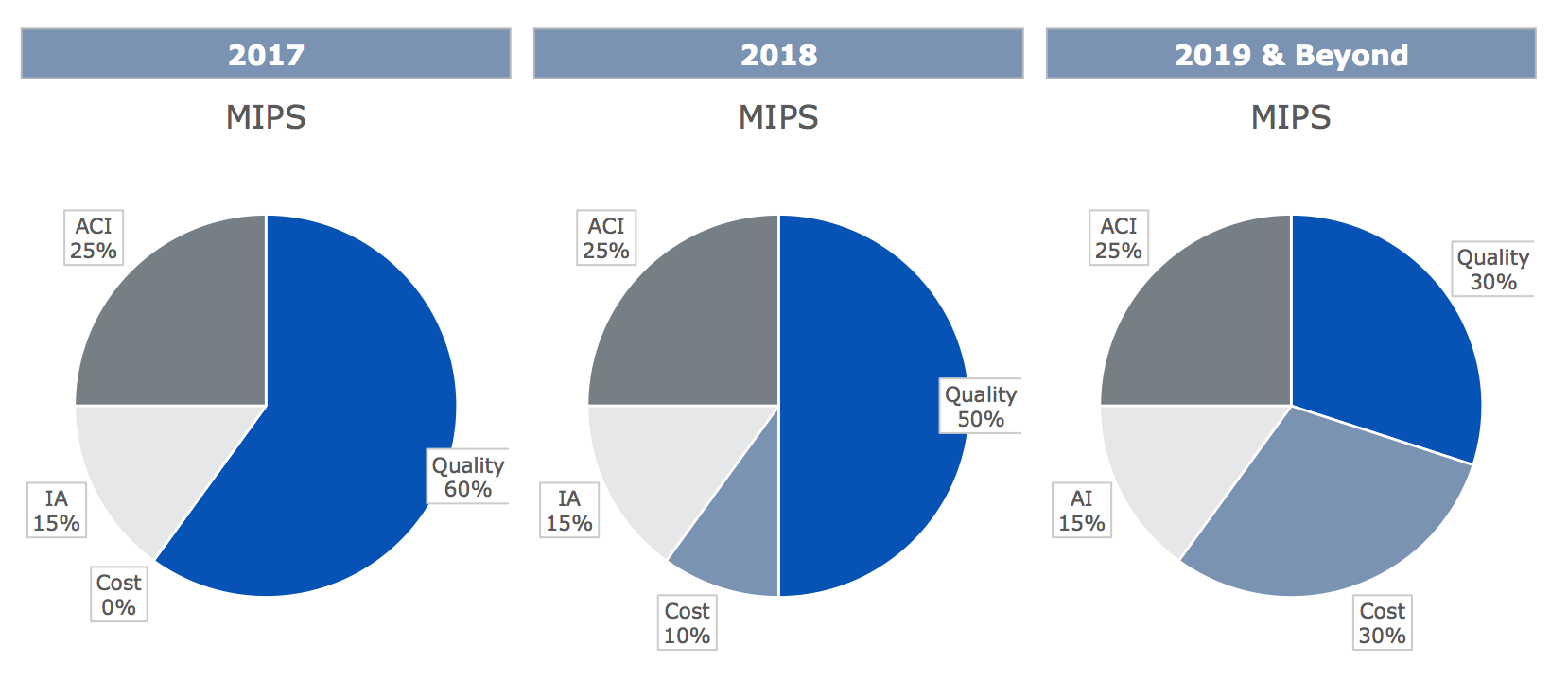 Notice that cost will slowly but surely consume weight devoted to quality today until they are equally weighted in 2019…sure hope they get it right!
Notice that cost will slowly but surely consume weight devoted to quality today until they are equally weighted in 2019…sure hope they get it right!
Payment adjustment
As a reminder, 2017 is considered a transition year. It takes very little work this year to avoid the 4% MIPS haircut in 2019. If you obtain 3 points from any of the MIPS categories this year, you will not incur a penalty in 2019. The stakes are a little higher next year. The work you do within MIPS next year will impact your 2020 Medicare fee schedule. It will be a little more difficult to avoid the 5% maximum MIPS penalty in 2020. To avoid that penalty, you must accumulate at least 15 points across the four MIPS categories that are scored in 2018. On a positive note, the potential upside for 2020 rises to at least 5% for those who outperform the nation in MIPS.
Performance period
One minor change, but worth highlighting, is the measurement period varies for the four categories of MIPS. Cost and quality are measured for the entire 12 months in 2018, whereas advancing care information and improvement activities will continue to only require a continuous 90-day period of measurement.
Small practices
On a positive note, small practices will see new benefits in 2018. The MIPS definition of a small practice is a TIN with 15 or fewer NPI numbers (don’t forget to count your advanced practitioners). CMS is clearly focused on making life easier for docs in small groups, and most of the nephrology practices in this country are in this bucket. Many of the benefits extended to small practices in 2017 are carried over into 2018. In addition to the current benefits, the final rule adds the following:
- Providers in small practices will collect five MIPS points simply for practicing in a group with 15 or fewer providers
- Raising the low-volume threshold (noted above) is advertised as a small practice win—just not one for nephrology practices
While not a small practice benefit, new for 2018 is a complex-patient bonus. As you may recall, the proposed rule pointed out that nephrologists care for “sicker” patients than the rest of medicine. The HCC score for Medicare beneficiaries cared for by nephrologists exceeds 3.0. Our efforts in caring for complex patients will be rewarded next year with up to five additional MIPS points.
Advanced APMs
The 2018 final rule offers little change to the AAPM track of the QPP that would impact nephrologists next year. The rule did reiterate CMS’ expectation that the number of Qualifying Participants (QPs) in an Advanced APM would increase to between 185,000 to 250,000 eligible clinicians in 2018. Recall these individuals are excluded from MIPS and will collect the 5% AAPM bonus in 2020. The AAPM that’s most relevant to nephrologists is the ESCO.
While not relevant in 2018, they go to great lengths to unpack the approach to incorporate payers in the “All-Payor Combination Option”, in order to determine QPs in 2019 and beyond. This will create additional flexibility as the QP hurdle rises in future years. Perhaps a topic for a future blog post?
Summary
As a numbers guy, I couldn’t help but notice there are fewer words in this blog post than pages in the final rule. I count 49 days until we ring in 2018. The QPP is here to stay, and as anticipated, the MIPS side of the program will become increasingly challenging as the program matures. Little has changed since Diana’s exceptional review of the proposed rule was posted. I hope today’s post helps you begin to sort out 2018. I am certain the Acumen blog will revisit this rule between now and the end of the year.
Of interest, this was published as a final rule with comment period. Do you have comments about the 2018 QPP? If so, you could send them to CMS, but it is more fun to share them with the Acumen blog. Join the conversation and drop us a note. And if you are a hoops fan, enjoy the game tomorrow night!
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Image from www.canstockphoto.com




Leave a Reply