 February! The NFL season is over. Did your team win last night? Did you enjoy the commercials? Perhaps you are not a sports fan and are delighted the football craze is behind us. Regardless of your level of interest in football, as a nephrologist entering year 3 of the QPP, you are facing your first taste of the impact the QPP will have on your Medicare physician fee schedule. It’s been a while since we have had a lyric-based post, but since the fee schedule is all about money, it’s time to fill that void.
February! The NFL season is over. Did your team win last night? Did you enjoy the commercials? Perhaps you are not a sports fan and are delighted the football craze is behind us. Regardless of your level of interest in football, as a nephrologist entering year 3 of the QPP, you are facing your first taste of the impact the QPP will have on your Medicare physician fee schedule. It’s been a while since we have had a lyric-based post, but since the fee schedule is all about money, it’s time to fill that void.
Money, get away
Unlike the opening line in this classic from the early 70’s, you can’t get away from the QPP. As a quick reminder, the QPP, which began in 2017, divides providers into those within an Advanced Alternative Payment Model (APM) and those who are exposed to the Merit-based Incentive Payment System (MIPS). If you were a Qualifying Participant in an Advanced APM in 2017, you can stop reading and either return to basking in the glow of a super bowl victory or wondering how such a promising season slipped away at a most inopportune time. Either way, sometime this year, you will collect a lump sum payment equivalent to 5% of your 2018 Part B book of business. Not a bad deal even if your team suffered the agony of defeat. For those of you in the MIPS path, the remainder of this post is for you.
Money, it’s a gas
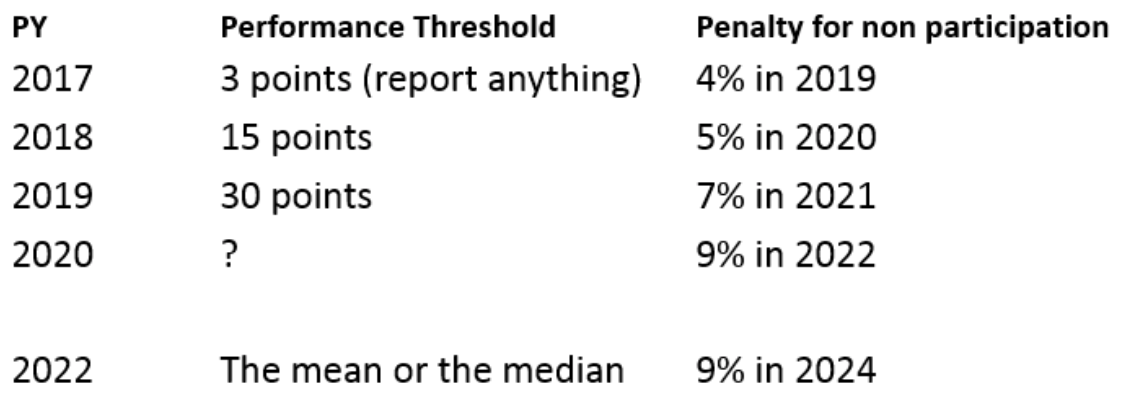
Whether it’s a gas or not may be a matter of perspective. Take a look at what used to be one of my favorite MIPS-related images below:
This is graphical view of the anticipated impact MIPS would have on your fee schedule, created by the Advisory Board a few years ago. To orient you, imagine the horizontal axis is your MIPS score with 0 (“I ignored MIPS and did not play”) on the far left and 100 (“I crushed MIPS with a perfect score”) on the far right. Turn your attention to the green line, which was expected to describe what would happen to your 2019 fee schedule. The original plan was to line up every doc left to right from lowest to highest MIPS score. That vertical dashed line in the middle of the chart labeled threshold score? That was intended to be either the mean or the median MIPS score from across the country.
Suppose for the sake of example, that threshold score was 50 for calendar year 2017. This was how it was supposed to work. You score a 50 in 2017 and CMS would levy a 0% adjustment on your fee schedule in 2019 (i.e., you face no penalty). Score below 50 and you would face a negative adjustment to your fee schedule this year. And if you scored lower than 25% of the threshold score in 2017, you would incur the maximum penalty in 2019 and see your fee schedule cut by 4%. Score above 50 in 2017 and you were supposed to receive the 2019 fee schedule with a positive adjustment (a bonus). As a budget-neutral program, the size of that bonus is dependent on how much money CMS collects from those to the left of the threshold score. At the outset of this program, there was talk that those who scored a perfect 100 would receive at least a 4% bonus, and with a scaling factor it could be as high as a 12% bonus!
Money, get back
Well, a funny thing happened when the rubber met the road. In an effort to ease the medical community into the program, CMS created the concept of a transition year for 2017. This basically meant if you made a minimal attempt to participate in MIPS, you would not be penalized. In essence, they postponed the requirement that the performance threshold was either the mean or the median. Instead, for 2017 they fixed the performance threshold at 3 points. That’s right, score 3 out of a possible 100 points and you face no penalty.
Money, it’s a hit
It certainly is a hit! What’s the real impact of migrating away from the intended approach and setting the performance threshold so low? Well, perhaps most importantly, it means very few 2017 participants will face a penalty in 2019. In fact, based on a recent review of the numbers posted in a Health Affairs blog referenced below, only 5% of the nation’s MIPS eligible clinicians will face a MIPS-related fee schedule reduction this year. Of course, the “bad news” is that with so few folks facing a penalty, this budget-neutral program had very little money to hand out in the form of bonuses. In fact, those at the very top of the MIPS scale in 2017 are not receiving a 12% bonus in 2019, nor are they receiving a 4% bonus. Those with a perfect MIPS score in 2017 will receive a 1.88% bump on their PFS in 2019.
Money, it’s a crime
Crime may be a bit harsh, but the approach is certainly misleading to say the least. CMS created this “problem” by establishing a very low performance threshold instead of using the national mean or median score as originally intended. What, you may ask, were the 2017 mean and median MIPS scores? 79 and 84 respectively. Think about that for a moment. We have a program where the original cut point that separates those facing a penalty from those collecting a bonus was supposed to be in the low 80s, but the actual cut point is 3. Perhaps it is a crime?
Money, so they say
No, money is not “the root of all evil today,” but when that lyric rolls off David Gilmour’s tongue…well, I digress. I think it is very important for everyone to realize the impact that fixing the performance threshold has on the MIPS program. Take a look at the table below. Based on my read of the final rule, the performance threshold will be fixed at least through this performance year, and it may not default to the national mean or median until performance year 2022.
It’s no surprise that they’re giving none away
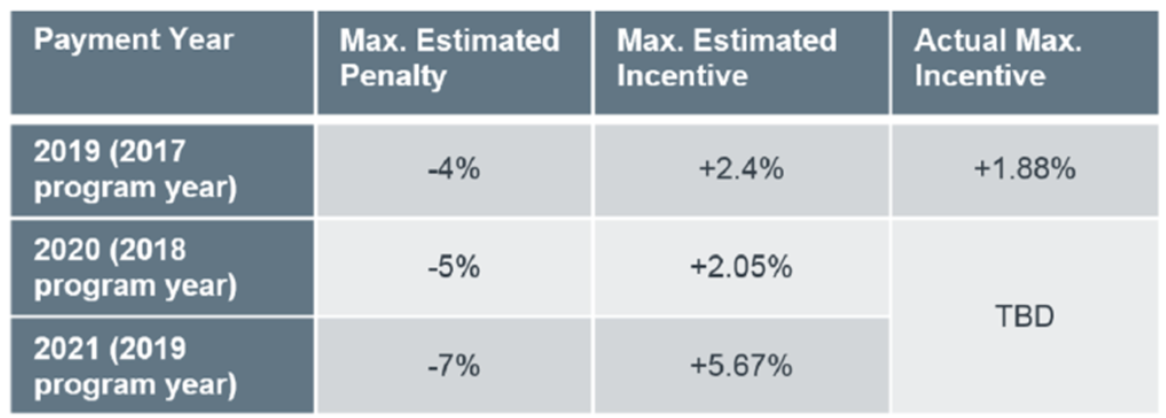
Wiser words were never spoken. There is no free meal at the MIPS table. Check out the table below, again from the advisory board:
By artificially fixing the performance threshold well below what’s likely to be the mean or median, CMS is both limiting the number of MIPS providers who will face a penalty, but also limiting the upside for those who crush MIPS. I think this is good news for nephrology practices exposed to MIPS. But last month Amol S. Navathe and colleagues wrote an exceptional blog post in Health Affairs raising some interesting points to the contrary. That post is well worth your time and attention.
Think I’ll buy me a football team
Sports fan or not, MIPS is obviously not intended to front the down payment for your entrée into the owner’s box. But setting the proper expectation for your practice will likely go a long way towards creating practice bliss. While the practice of medicine has never been about money, most of you are operating businesses and must keep your eye on the ball. The MIPS program has more nuance than a band from the 70s whose album spent more time on the Billboard 200 than any other album on the planet. We will keep digging, but if the answers to your MIPS questions are not within the Acumen blog, perhaps we should search for them on the Dark Side of the Moon.
Do you have thoughts about setting a low performance threshold? Drop us a note and join the conversation.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Image from www.canstockphoto.com




Leave a Reply