 Happy President’s Day! What does one do on President’s Day anyway? If you aren’t lucky enough to have the day off, maybe you can spend President’s Day thinking about the Government – more specifically, the Centers of Medicare and Medicaid Services (CMS). Because it’s that time of year to submit your 2017 data for the Merit-based Incentive Payment System (MIPS).
Happy President’s Day! What does one do on President’s Day anyway? If you aren’t lucky enough to have the day off, maybe you can spend President’s Day thinking about the Government – more specifically, the Centers of Medicare and Medicaid Services (CMS). Because it’s that time of year to submit your 2017 data for the Merit-based Incentive Payment System (MIPS).
Clinicians must attest by March 31st, 2018, to avoid a -4% payment adjustment in 2019!
Decisions, decisions!
Submitting your data may be as complicated as the MIPS program itself! There are so many decisions to make and things to do before you are ready to attest.
If you don’t believe me, these are just a few high-level questions you should be asking yourself:
- Do you need to submit MIPS data?
- Are you excluded?
- Are you considered a Qualifying Participant (QP) in an Advanced Alternative Payment Model (AAPM)?
- Are you a part of a MIPS Alternative Payment Model (APM) that will submit data on your behalf?
- Are you submitting as an individual or a group?
- What pace will you pick?
- Submit data for the entire 2017 calendar year (the most competitive option).
- Submit data for at least a 90-day period within 2017.
- Submit “something” (the minimum to avoid a penalty).
- For Advancing Care Information (ACI)…
- Will you take a hardship?
- What edition EHR are you using? (Acumen customers will choose 2014 edition.)
- What is your reporting period?
- Did you meet all the base measure requirements?
- What performance measures will you report?
- Are you eligible for any bonus points?
- Do you have a copy of your performance dashboard in case of an audit?
- Do you have supplemental documentation on file in case of an audit? (Hint: make sure to do a security risk analysis!)
- How will you submit your ACI data?
- For Improvement Activities…
- What activities did you select?
- Did your practice complete these activities for a minimum of 90-days?
- Do you have the correct documentation on file in case of an audit?
- How will you submit your improvement activity data?
- For Quality…
- What quality measures did you select?
- What is your reporting period?
- If you are not taking the “submit something” path…
- Did you choose at least 6 measures (or a specialty set)?
- Take a look at the published benchmarks to decide which 6 are the most competitive.
- CMS will accept more than 6 measures and will score you on the top 6 measures.
- You must report on at least 50% of the patients that meet each measure’s population definition.
- Did you select at least 1 outcome measure?
- Did you choose at least 6 measures (or a specialty set)?
- How will you submit your quality data?
For those that have no clue about any of the items above, there is always the “submit something” path to avoid a penalty!
If you are still with me, read on.
Multiple pathways
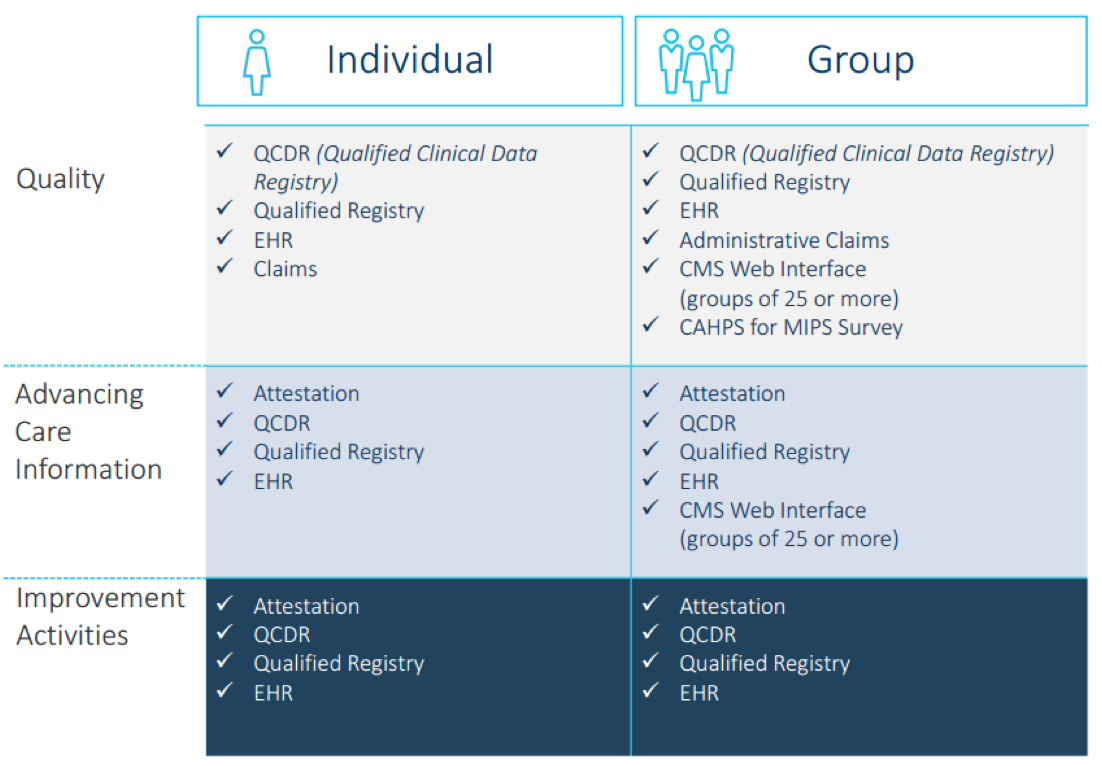
There are multiple pathways to submit your MIPS data to CMS. The submission mechanisms available to you depend on:
- Whether you are reporting as an individual or as a group;
- The size of your group;
- The type of health information technology you use;
- The performance category on which you’re reporting; and
- Whether you participate in an MIPS APM or Advanced APM.
To further complicate things, you do not need to choose the same data submission method for each category under MIPS!
Take a look at the image below. By now you should have a good idea on what method you will select under each category.
For most clinicians who are reporting individually, I am going to assume that the majority will do the following:
- Quality: manually upload a QRDA cat III XML (generated by your EHR) into the QPP submission website
- Advancing Care Information: manually attest via the QPP submission website
- Improvement activities: manually attest via the QPP submission website
Disclaimer: Every situation is unique. You may be set up with a third-party tool (such as a Qualified Clinical Data Registry) or be part of a group/APM that will submit data on your behalf.
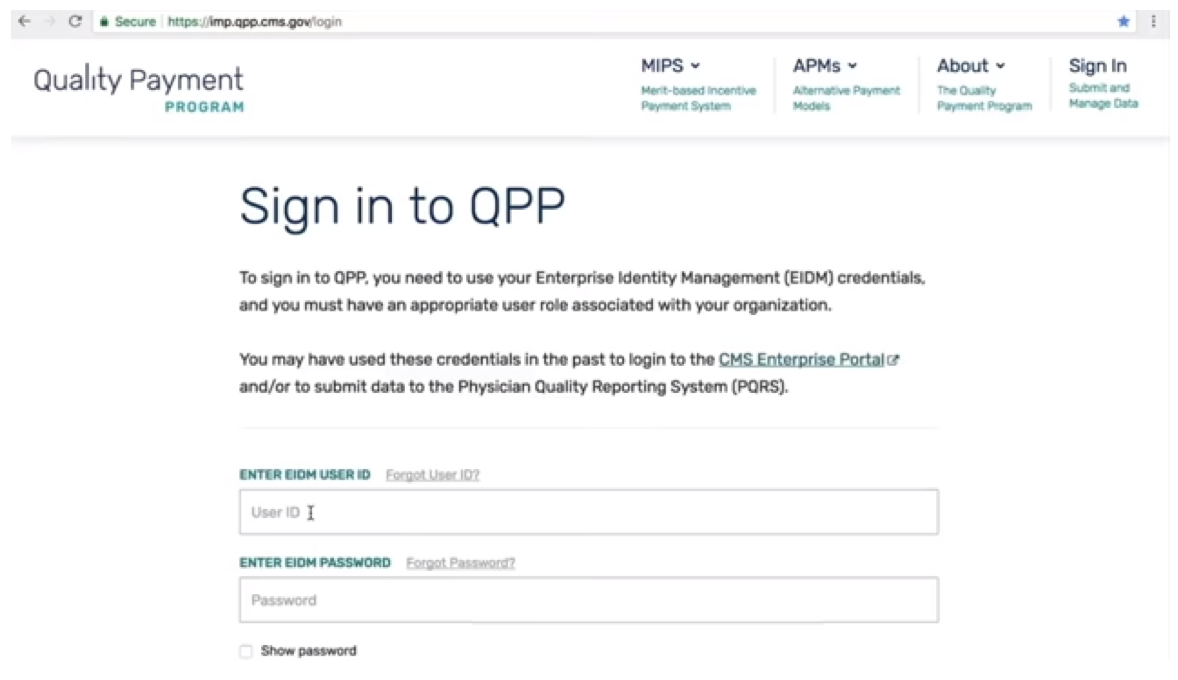
Set up your EIDM account
If you plan on manually attesting to any category of MIPS, or if you plan on uploading your quality data, you must have an Enterprise Identity Management (EIDM) account. This will be required before you can sign into the QPP system for data submission.
You can set up an EIDM account via the CMS Enterprise Portal. You will need to select an appropriate user role associated with your organization. For example, a practice manager may set his/herself up to submit on behalf of clinicians in the practice.
An EIDM account can be a bit tricky to set up – so get an early start!
Ready to submit?
So, you are ready to enter your data now, right? NOT SO FAST! One mistake I often see practices make is to forget to prepare an audit folder. CMS can request an audit up to 7 years after you submitted your data! If you don’t know what to have on file, take a peek at the PDFs found in this Zip file. The file also contains a PDF on suggested documentation for improvement activities, which is very helpful.
OK, now you are ready!
Now that you have all your information collected, you can log into the QPP site to submit data.
The QPP system is set up like a wizard in that it will walk you through each question one at a time to ensure you don’t miss a step.
The QPP system will score you in “real-time” so you understand how well you are doing in the program. It quantifies scores based on clinician submissions as data is being entered into the system. If you are submitting a quality measure without a benchmark, you will see the benchmarks change during the submission window as more clinicians submit data for that measure.
I highly encourage you to log into the QPP system early and often to familiarize yourself with the data submission and scoring method. You can update information as often as you like. CMS will use the last data update before March 31 as your final submission.
Lastly, before you attest, take a minute to read this fact sheet along with watching a 38-minute YouTube video posted by CMS about data submission. These are fantastic resources.
Good luck!
Important MIPS Resources
- Data Submission Fact Sheet
- CMS Data Submission YouTube Video
- QPP Helpdesk: 1-866-288-8292 or email qpp@cms.gov.
- QPP Resource Library
- EIDM guide
- Quality Payment Program (QPP) Data Submission Feature
- CMS Enterprise Portal
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Image from www.canstockphoto.com





Leave a Reply