 Can you believe it will be Christmas Eve in 2 weeks? Have you finished your holiday shopping? I certainly have not. As you consider those trips to the mall or surfing the Internet to find just the right gift to purchase, let’s spend some time today exploring how our good friends at CMS think about cost. Today we are going to unpack one of the most confusing aspects of MIPS: the cost performance category. Are you ready to review what’s in store for 2019? You may enjoy this even more than trying to find a parking spot at the mall this week!
Can you believe it will be Christmas Eve in 2 weeks? Have you finished your holiday shopping? I certainly have not. As you consider those trips to the mall or surfing the Internet to find just the right gift to purchase, let’s spend some time today exploring how our good friends at CMS think about cost. Today we are going to unpack one of the most confusing aspects of MIPS: the cost performance category. Are you ready to review what’s in store for 2019? You may enjoy this even more than trying to find a parking spot at the mall this week!
Weight
As Diana noted in her fantastic summary last month, for 2019 Cost will be worth 15% of your total MIPS score, up from 10% this year. That extra 5% comes from Quality which drops from 50% this year to 45% in 2019. As you may recall, the original plan was for cost to jump to 30%, placing it on equal footing with quality which was scheduled to drop to 30%. Organized medicine was none too happy about that abrupt change, and to their credit, CMS took note. While yours truly would have been happier with a repeat at 10% next year, the gradual rise to 15% is certainly better than what was originally contemplated. Within the final rule, CMS mentions they will finalize the cost category weighting for future years in future rule making. However, they have hinted at their intent to bump cost by 5% per year until they reach the 30% figure for MIPS payment year 2024 (performance year 2022).
Data submission
This is just about the easiest part of this blog post to write. Just like this year, next year the cost performance category will be harvested from administrative claims data. That’s right holiday shoppers, neither you nor anyone in your practice need lift a finger to make this happen. CMS measures this in the background, which may be both a blessing, and a curse.
The measures
With the easy stuff out of the way, it’s time to roll up our sleeves and look under the hood. There will be 3 cost measures in 2019:
- Total per capita cost (TPCC) measure
- Medicare spending per beneficiary (MSPB) measure, and
- Episode-based measures, which are new for 2019
To make this just a little more complicated, the rules of engagement for each of the 3 measures within the cost performance category are different. Each has its own unique attribution scheme, resulting in variable impact upon nephrologists. Each cost measure has specific case minimums, and of course, the definitions of the actual measures will create variable impact on the practice of nephrology. Within this context, let’s take a look at each measure individually.
Total per capita cost
This measure is unchanged for 2019. As the name implies, TPCC determines the total Part A and B costs for Medicare patients attributed to the provider. Best way to think about TPCC is to consider the following fraction:
The annualized, risk-adjusted, specialty-adjusted Part A & B costs incurred by all attributed patients
________________________________
The number of Medicare patients attributed to the provider
Note with MIPs, you can report as an individual or as a group. Above I am showing the scheme for an individual. Practices electing to report as a group are calculated in a similar fashion, but the cost measures are rolled up at the group level.
The tricky part here in my view is the attribution scheme. Only one provider is held accountable for each patient with respect to TPCC. Attribution follows a 2-step process focused on the delivery of “primary care services” defined by specific CPT codes (largely outpatient E&M codes). CMS is basically looking for the provider that delivers the largest number of primary care services to the patient over the course of the year. If that’s you, the patients Part A and B costs are added to the numerator above, and you increase the denominator by one.
- First, CMS looks for primary care services delivered by primary care providers. For this measure a primary care provider is either a general practioner, family practioner, general internist, geriatrician, clinical nurse specialist, nurse practioner, or physician assistant.
- If the Medicare patient does not receive a primary care service from a primary care provider during the year, they next look for evidence of primary care services (same E&M codes as in step 1) delivered by specialists, like nephrologists.
Bottom line, if your NPs or PAs deliver primary care services, billing with their NPI, there’s a decent chance they could end up in the TPCC bucket. The other way nephrology practices get tagged by TPCC is if your ESRD patients have no primary care services with primary care, but you perform them in an office setting. Both of these strike me as rare events, but they could happen. Our last saving grace with respect to TPCC is the minimum case load. Each individual provider must have at least 20 patients attributed during the year in order for this measure to count.
Medicare spending per beneficiary
As with TPCC, nothing changes for MSPB in 2019. Unlike TPCC, I think there’s a good chance nephrologists will get tagged by MSBP. MSBP is basically measuring costs incurred during and immediately after an inpatient stay. For this measure, the clock starts ticking 3 days prior to admission and it runs through day 30 post discharge. Add up all the Medicare Part A & B costs incurred during the time window, and you basically have the Medicare spending per beneficiary.
The attribution scheme employed for MSBP is important for us to understand. CMS is basically adding up all Part B services provided during the index hospital stay, and they are looking for the doc who delivered the plurality of those services. If that’s you, this MSPB is yours. Imagine the Part B services delivered to your dialysis patients during a hospital stay. If your Part B services exceed those of any other provider seeing the patient in the hospital, tag you’re it!
MSPB is risk adjusted in a similar fashion to TPCC, but unlike TPCC, this one is not specialty adjusted, which means for MSPB we are “competing” with all provider types. The minimum case load for this one is 35. If the attribution scheme above occurs 34 or fewer times during the year, you are not held accountable for MSBP. Clear as mud, right?
Episode-based measures
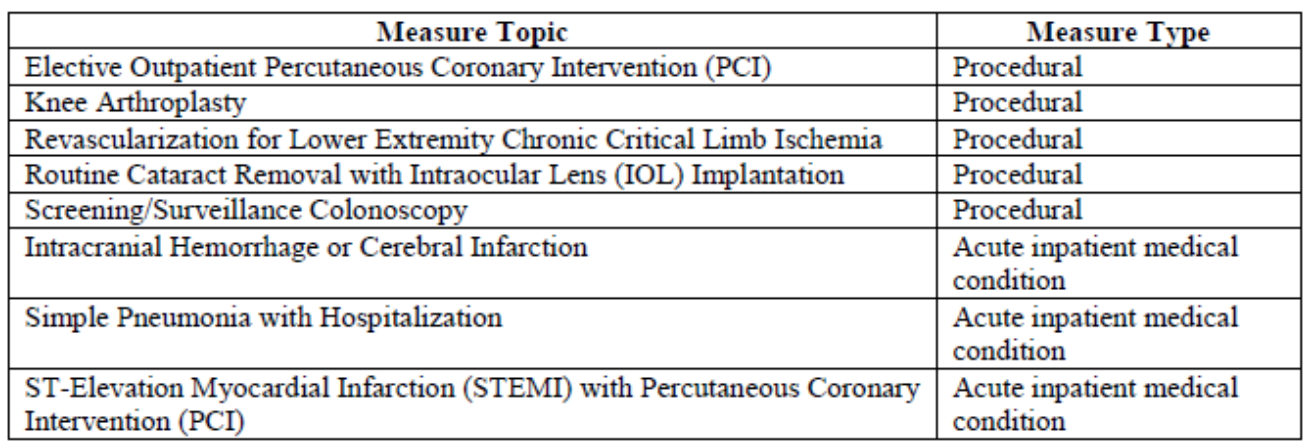
The new kid on the block is the episode-based measures. These have rightfully garnered quite a bit of negative attention by organized medicine, but in spite of that, CMS is releasing 8 of these next year. The measures are considered either procedural (the episode is triggered by a specific procedure) or they are defined by a specific inpatient medical diagnosis. The table below highlights the 8 episodes in play for 2019.
While these measures will not typically apply to nephrologists, additional measures are under development for future years, and we should pay close attention to how these things work.
Of interest, each of these episodes have very detailed specifications that highlight how the episode is triggered, how long the episode lasts, and what costs are included in the episode. Like the MSPB and TPCC measures, episode-based measures also have a minimum case load. The minimums are 10 cases for the procedural episode-based measures, and 20 cases for the acute inpatient medical condition measures.
The attribution scheme for episode-based measures varies by measure type. And while our specialty is not in the crosshairs for 2019, the scheme in play for the medical condition episodes would keep me up at night. The procedural episodes are basically handed to the doc performing the procedure. For the acute inpatient medical condition episodes, it’s a little scary. CMS intends to look at all of the E&M services provided to the patient during the trigger inpatient stay that defines the episode. If you are a doc with a claim billed using a TIN that renders at least 30% of the inpatient E&M claim lines during that hospital stay, the episode is attributed to you and every other doc with a claim using that TIN during the inpatient stay. Think about this for a moment. If you are on call over the weekend, covering your partner’s patients, you could get tagged with one of these episodes, even though your impact on the cost of that episode is nonexistent!
Scoring
If you are still reading 2 weeks before Christmas Eve, hang in there, we are close to home. Scoring is reasonably straightforward. Benchmarks for all 3 measures within the cost category are determined during the measurement year. If you meet the case load minimums for all 3 measures, each measure contributes equally to your cost score. If you only have enough cases to meet the minimum for one of the 3, that becomes your cost score. Finally, as with 2018, if you don’t meet the case minimum for any of the 3 measures, your cost category is reweighted to zero, and the 15 cost points move to quality, making quality worth 60% of your overall MIPS score.
Cost
I find the cost category to be the most confusing category within MIPS. I also believe it is the most difficult category to impact. It is now on equal footing with the improvement activities category, and in a few short years, cost and quality will be equally weighted, and together worth over half of your total MIPS score. I doubt we will see much impact for nephrology in 2019, but we should pay very close attention to the cost category as CMS releases additional episode-based measures in the years ahead.
I hope you enjoy your holiday shopping. As you search for those prime parking spaces at the mall, the Acumen blog will continue to search for answers to the QPP. If questions arise, drop us a comment. Happy holidays from all of us at Acumen.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Image from www.canstockphoto.com




Leave a Reply