 We’re halfway through July and 72 days from the ICD-10 transition (yes, I am counting). The days are long and hot and some of us occasionally have trouble falling asleep at night. For those of you with insomnia, that annual summertime cure arrived about 10 days ago. Yes, the proposed rule for the 2016 Medicare physician fee schedule was released on July 8. Weighing in at a slumber-inducing, 815 double-spaced pages, there are a few nuggets of interest for us within the pages of this tome. The shorter—though, in my opinion, more difficult to read—official version of this notice of proposed rule making (NPRM) was published in the Federal Register on July 10. As part of our review of the NPRM, let’s examine the new Merit-based Incentive Payment System, thankfully shortened to MIPS.
We’re halfway through July and 72 days from the ICD-10 transition (yes, I am counting). The days are long and hot and some of us occasionally have trouble falling asleep at night. For those of you with insomnia, that annual summertime cure arrived about 10 days ago. Yes, the proposed rule for the 2016 Medicare physician fee schedule was released on July 8. Weighing in at a slumber-inducing, 815 double-spaced pages, there are a few nuggets of interest for us within the pages of this tome. The shorter—though, in my opinion, more difficult to read—official version of this notice of proposed rule making (NPRM) was published in the Federal Register on July 10. As part of our review of the NPRM, let’s examine the new Merit-based Incentive Payment System, thankfully shortened to MIPS.
Origins
MIPS is brought to you by MACRA—the Medicare Access and CHIP Reauthorization Act of 2015. (Thank God for acronyms!) You may not recognize MACRA, but this piece of legislation was the toast of the town earlier this year, as it laid our old friend the SGR to rest. Of course, that’s not all MACRA did. In an honest effort (I think) to make our lives easier, MIPS was created to roll up the disparate CMS incentive programs that exist today.
As of January 1, 2019, there will no longer be a requirement to report PQRS or attest to Meaningful Use or worry about the thing none of us truly understands—the Physician Value-based Payment Modifier. No, in just a few short years our lives will be simpler, as these three programs are rolled up into MIPS. At least, that’s the plan.
Who is in?
What’s clear from the NPRM is this program will largely be administered at the individual provider or NPI level as opposed to the practice or TIN level. CMS plans to start with the usual suspects in 2019 and 2020 when MIPS will be applied to the following eligible professionals:
- Medicare physicians, which include MDs and DOs, dentists and oral surgeons, podiatrists, optometrists, and chiropractors
- PAs, NPs, and CNS (clinical nurse specialist)
- CRNAs
In 2021 and beyond all providers listed in section 1848(k)(3)(B) of the Social Security Act are in. This is basically every provider with an NPI number.
What else is in the NPRM?
There is remarkably little detail in this proposed rule about MIPS, but a few things are clear from the NPRM:
- There will be a low-volume threshold for participation. While the number is not fixed in stone, the NPRM has tossed out a figure of 10%. (If less than 10% of your patient encounters occur with Medicare Part B beneficiaries, you would not be subject to MIPS.) This figure provides no quarter for the typical nephrology practice.
- There is a lot of uncertainty as to what may constitute “Clinical Practice Improvement Activities” but the act requires that this section of MIPS include at least the following subcategories which look remarkably similar to the National Quality Strategy domains we have previously reviewed:
- Expanded practice access (make it easier for patients to see you)
- Population management
- Care coordination
- Beneficiary engagement
- Patient safety
- Participation in alternative payment models
- They will soon issue a request for information, which will be designed to assist them with the task of filling in some of the blanks.
There must be more!
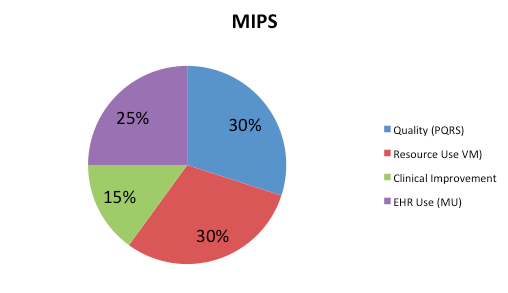
I must say I was a bit underwhelmed at the paucity of insight related to MIPS present in this NPRM, but if you stuck with this otherwise sleepy post, you are in for a treat. MIPS will create a composite performance score for every eligible professional. That score consists of four components, each weighted differently as noted in the pie chart below. The Advisory Board suggests that in 2019 quality will be weighted at 50% with resource use weighted at 10%. According to the Advisory Board the pie chart below represents the mix for 2021 and beyond.
Figure 1: MIPS Category Weights
Your MIPS score is a number between 0 and 100, and believe me when I say in this game you’d prefer to be as close to 100 as possible. What’s proposed is the following: During a benchmark year (which my guess will be 2017) every provider in the country will be scored. Next, the mean or median (depending on which is chosen) of the nation’s providers will be determined. That figure becomes the performance threshold. If your MIPS performance score exceeds the threshold, congratulations! Your Medicare Part B fee schedule will be higher than what’s published. On the other hand, if your score is below the threshold, expect a haircut on your entire Part B book of business.
How much?
This is where things really get interesting. If your score is less than 25% of the performance threshold, the hammer comes down and you will face the maximum MIPS penalty. If your score is 25-99% of the threshold, you face a linearly declining penalty. The closer you are to the threshold the lower your penalty. If your score is identical to the performance threshold, you face no penalty. If your score exceeds the threshold, your “bonus” rises in a linear fashion, increasing as you climb higher above the threshold. Compared to the individual programs in place today, this is a very stout incentive program. Check out the maximum penalties and the possible bonus one may face with MIPS in the table below:
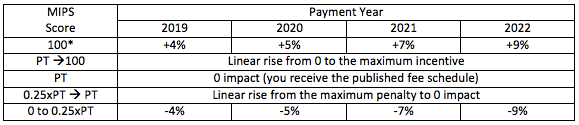
Table 1: MIPS payment adjustment. *Maximum bonus is multiplied by a scaling factor to achieve budget neutrality (could be as high as 3x). PT = Payment Threshold, which is the mean or median national score during the measurement year.
Note as with the value-based payment modifier, MIPS is a budget-neutral program. The number of dollars collected from the providers below the performance threshold will determine the scaling factor for the bonus. The scaling factor can be as high as 3x. If that happens in 2022 the Medicare fee schedule for docs with a MIPS score of 100 will be 36% higher than those docs who receive a goose egg for MIPS! We have never seen a program with the potential for this much spread.
Alternative payment models to the rescue?
As daunting as MIPS appears today, there is another—and many believe preferred—path. In an effort to steer providers to alternative payment models, providers who receive a “significant” amount of their revenue from alternative payment models will not only avoid MIPS, but they will collect a 5% bonus on their Part B book of business. The details remain a bit murky and I suspect clarity will arrive in next year’s proposed rule, but many are suggesting “a significant amount” is 25%. So if in 2019 and 2020 you receive 25% of your Medicare revenue via an alternative payment model, you don’t have to play the MIPS game and you will collect the 5% fee-for-service bump for having skin in the game via one of the alternative payment models.
Asleep at the wheel
Over the past few years the folks at the Acumen blog have invested a lot of time and effort to help spread the word regarding the impact multiple CMS incentives have upon the nephrology community. In a few short years the big three will formally ride off into the sunset, as 2018 will be their last year. What’s taking their place, however, is a remarkably important synthesis of quality reporting, resource utilization, meaningful use, and an as yet to be determined measure of clinical practice improvement. MIPS is very clearly not the preferred path as CMS would like to see everyone participating in an alternative payment model. The reality, however, is that physicians practicing in rural communities and certain specialists may not have alternative payment model opportunities. It is this group of providers for whom MIPS was created.
Don’t fall asleep at the wheel. Pay close attention to MIPS as it could prove to be the most impactful CMS program to date.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.




Leave a Reply