 Can you believe that we only have a few months left of using the term “Meaningful Use” before it’s retired? There’s a small (and I mean small) part of me that will mourn the loss of the term—mainly because it’s easier to say than its successor, “Advancing Care Information.”
Can you believe that we only have a few months left of using the term “Meaningful Use” before it’s retired? There’s a small (and I mean small) part of me that will mourn the loss of the term—mainly because it’s easier to say than its successor, “Advancing Care Information.”
Therefore, I will take this small window of opportunity to use the term as much as I can until it meets its demise.
A quick rundown of your objectives
Unlike next year, Meaningful Use still remains an all-or-nothing program in 2016. This means that you must meet all of the requirements for each objective (unless you qualify for an exclusion) in order to avoid a negative 3% payment adjustment in 2018!
In 2015, CMS drastically changed the MU objectives by retiring a lot of “topped out” measures and reducing thresholds for others. This left everyone with the following list of 10 objectives to meet regardless of stage.
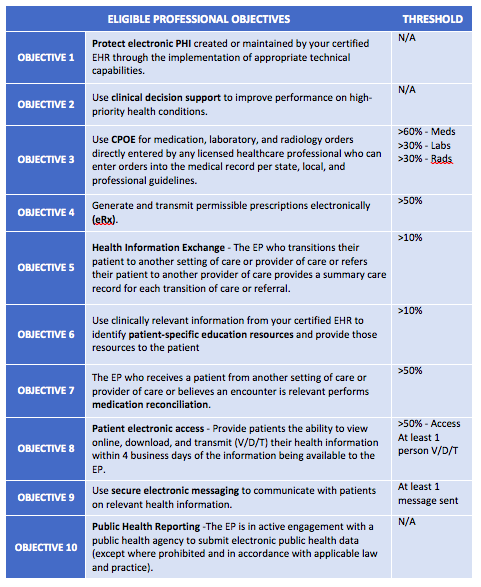
For more details on each objective, take a look here.
Another 90-day reporting period?
Earlier this year, CMS proposed changing this year’s MU reporting period from a full calendar year to any 90-day period. This seems to follow the trend of past years where industry groups pleaded for a little relief. Although the decision isn’t confirmed (we are waiting on the OPPS final rule), I would bet the proverbial farm that it will happen! So for those procrastinators out there, if the change goes through, your last possible start date would have been yesterday (October 2), so make today a good day of checking boxes!
For those who are in their first year of MU, you automatically get a 90-day reporting period in 2016.
Alternate exclusions
Another area of MU that has been causing a bit of confusion in 2016 is the term “alternate exclusions.” In 2015, CMS published a final rule that modified the MU program for years 2015-2017. In summary, they made one list of 10 objectives for everyone to follow (regardless of stage). In doing so, they realized that they would be making life harder for those providers scheduled for Stage 1. Therefore, they added alternative exclusions for certain objectives where there was not a Stage 1 measure equivalent.
This year, CMS removed all the alternate exclusions except for 2 (see beow). So if this year is your first year of MU, you don’t get it as easy.
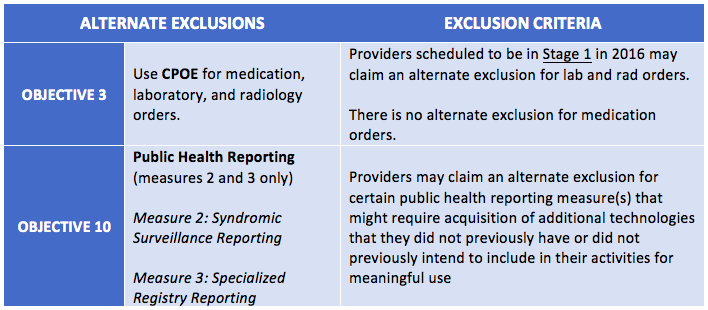
Be sure to take a closer look at the alternate exclusion for public health objectives. If you are a nephrologist, this one might be for you.
Pay attention to your performance
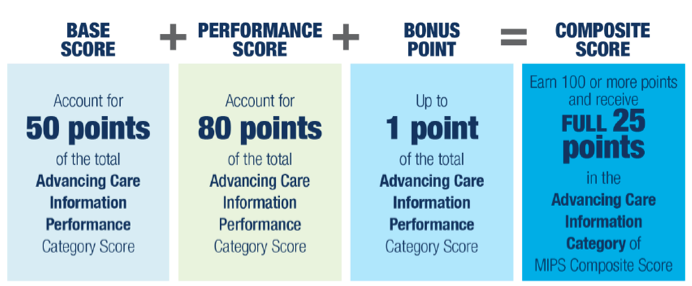
For our regular blog readers, you may recall that in order to get your full 100 points in the Advancing Care Information portion of MIPS next year, you will need to do well in certain measures.
The ACI category is made up of two main components—a base score and a performance score.
The base score is worth 50 points and is earned by simply reporting a numerator/denominator and yes/no attestations for the ACI measures.
The performance score portion is where you earn points based off of how well you do in certain measures. Although you can earn a possible 80 points, you only need 50 points to get a perfect score in the ACI category.
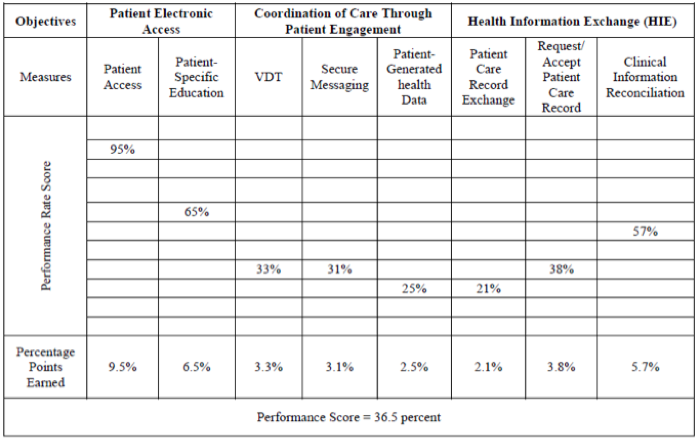
The best way to predict how well you will do in ACI next year is to look at how well you did on each threshold-based measure in 2016.
Each threshold-based measure could earn you a possible 10 points by dividing your performance percentage by 10. In order to get a full 10 points in one measure, you would need to get a perfect 100%. If you get a 90%, you would get 9 points…and so on.
ACI threshold-based measures and sample percentage scores
Did your measures add up to at least 50 points based on the formula above? If not, make it a new year’s resolution to strive to do better. Perhaps you can knock out the 50 points by only focusing on 5-6 measures, instead of having to tackle them all.
Hardship exemptions—a fan favorite
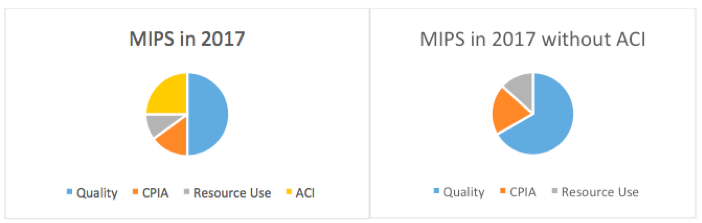
Don’t worry my friends, the hardship exemption option is still available and seems to be a very popular choice amongst nephrologists. It will be interesting to see if hardship exemptions are still popular next year. Taking a hardship in the new MU (ACI) will reweight your MIPS score adding more emphasis on the quality category.
Don’t lose focus
It’s very easy to get caught up in the whirlwind that is MACRA—but let’s not forget about what you need to do to finish this year strong. Understand how each MU objective works, protect yourself from an audit, understand your exclusions, know which measures to improve upon for next year, and make sure you report (or apply for a hardship) on time!
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Top image from www.canstockphoto.com




rg says
If I join an ESCO, do I still need to submit a meaningful use hardship exclusion in 2017? Or, does that not matter because I am in an ESCO. Thanks! RG
Diana Strubler says
Hey RG!
Being a part of the ESCO doesn’t escape you from MU that easily unfortunately. The proposed rule states that at least half of the providers in an ESCO should be using a certified EHR next year. It sounds like more than 50% of providers will need to qualify for the new MU in the office in order to qualify the ESCO.
I’d recommend taking a closer look at the final rule (expected in the next few weeks). Hopefully CMS removed (or eased) that part of the Advanced APM qualification.
Diana