The year is less than two weeks old and one question we have heard quite frequently is, How do we prepare for meaningful use in 2012? The answer is one that I grew tired of hearing during my days in business school: It depends.
Let’s walk through a couple of potential scenarios with the hope of clearing up some of the confusion. As a ground rule, I am going to assume that everyone is taking the Medicare path to meaningful use. The rules for the Medicaid approach are different.
You Attested Successfully in 2011
If you find yourself in this bucket, pat yourself on the back. You have the good fortune of facing the Stage 1 objectives for two more years (2012 and 2013). The principle difference this year and next is that the reporting period now expands to the entire calendar year. At first blush, this sounds a bit daunting, but in reality, you have already done the heavy lifting for the patients you see in follow up. For example, those patients should already have a problem on their problem list, demographics recorded and recently had their tobacco status updated. The other interesting nuance that results from expanding the reporting period to a full year is that the work you do in the dialysis facility becomes “less relevant” from a meaningful use perspective. By no means do I intend to imply the work is not relevant. It’s just “unique patient encounter” creates a scenario in which the encounter within the dialysis facility is marginalized as the reporting period expands because of the repetitive nature of our patient encounters in this venue of care.
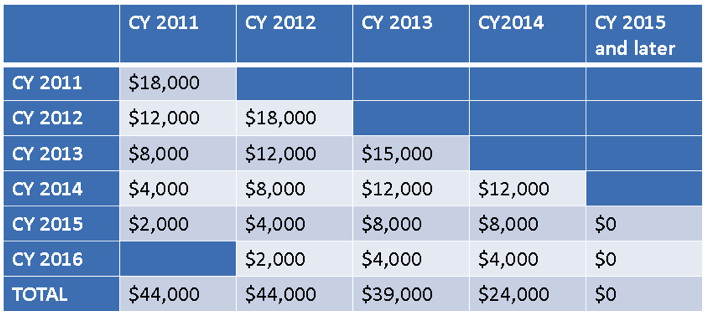
If you find yourself in this scenario, the year 2 incentive drops to $12,000. Further, the incentive will be paid following attestation, sometime in early 2013.
You Collected Data in 2011 but Have Not Attested
While I am quite certain no one reading this blog would ever procrastinate, I am equally certain you know someone who might. If you or someone you love captured the necessary data for meaningful use during a continuous 90 day period in 2011, there is still plenty of time to convey this to CMS. The 2011 attestation window closes on February 29, 2012. In fact, you can wait until the 28th of February to attest for 2011 and, at the same time, register to participate in 2012. However, I would not advocate waiting until February 28. Assuming you do attest for 2011 before the deadline, you will find yourself in the same bucket as the folks in the first scenario with regard to year 2 in 2012.
You Attested in 2011 but Have Decided to Sit out 2012
I doubt many folks will land here, but if you do, please be aware of the fact that you are potentially leaving incentive dollars on the table. Unlike the Medicaid path, the Medicare path to meaningful use is defined by the year you begin. The incentive is time stamped (the sooner you start, the more you can potentially collect). But the Medicare path also precludes recouping a skipped year’s incentive. If you are in this bucket and decide to return to the program in 2013, your potential incentive for 2013 is $8,000. The year 2 incentive ($12,000) has been lost.
Table: CMS EHR Medicare Incentive Schedule
2012 Will Be Your First Year to Attest for Meaningful Use
In this scenario, you face the stage 1 objectives this year and next. In addition, your reporting period in 2012 is any continuous 90 days. This provides you with the flexibility to begin your reporting period as early as January 1, 2012 or as late as October 1, 2012 (for your friends who procrastinate). As you may recall, CMS is paying the incentive within 6-8 weeks of successfully attesting. From a financial perspective, the earlier you attest, the sooner the incentive check arrives.
2013 Will Be Your First Year to Attest for Meaningful Use
This scenario similar to the scenario we just discussed, with a couple of caveats. Beginning the program in 2013 reduces the year 1 payment to $15,000, and the total incentive available to you over the course of the program drops from $44,000 to $39,000. You will face the stage 1 objectives during 2013 and 2014. Also, keep in mind that the first year you deal with meaningful use will coincide with the transition from ICD-9 to ICD-10. If you find yourself in this bucket, I recommend finishing the 90-day reporting period prior to October 1. From where I sit, you are tempting fate to include the transition date within your reporting period.
Do Not Forget to E-Prescribe
I know you will soon tire of hearing me refer to the eRx penalty, but I plan to continue to beat this drum until I wear it out. Regardless of which scenario you find yourself in, you need to do what it takes to avoid the CMS eRx penalty. Unfortunately, there is nothing you can do today if you are being penalized in 2012. But between now and June 30, 2012, try your best to send a script electronically during any encounter with ten Medicare Part B beneficiaries, put the eRx G-code on the claim you submit to Medicare and you should avoid the 2013 penalty (a 1.5% haircut on your entire Part B book of business).
Let us know if you have comments about the above, and we will post those here. Also, today I have a question for you. I am trying to determine how CMS intends to treat folks reporting year 2 of the Medicare meaningful use program in circumstances where they are not in the practice for the entire calendar year (e.g., a new doc joins the practice March 1 and he/she reported year 1 last year with the previous practice). If you know the answer or where to look, let us know by commenting here.


Peggie Lewis says
So if you are going to attest for MU in 2012 you just need to attest over a 90 day period. There seems to be some confusion about 90 days or the whole year. I am guessing it may be the whole years of 2012 and 2013 because you attested for 2011? Whereas those of us who attest in 2012 during the 90 days let’s say Sept 2012 to Nov 30, 2012 will have to start attesting for the whole year starting in 2013?
Terry Ketchersid, Vice President and Medical Officer at HITSG says
Peggie that is correct. There was a lot of confusion surrounding this early on but CMS has been very clear about this now. Basically regardless of which year the provider starts, the first year they attest, they will do so for a 90 day reporting period. For each subsequent year the reporting period is the entire calendar year. The unusual exception to this occurs on the Medicaid side of the program. There you can actually receive the year 1 incentive if you attest to the fact that you are adopting, implementing or upgrading a certified EHR. In that case the 90 reporting period occurs in year 2 and all subsequent years it is the entire calendar year.