 The Monday after Thanksgiving. Festive celebrations with family, large meals, a bit of football, and perhaps some shopping on Black Friday are all now in the rearview mirror. It’s Monday and we are left with, well, leftovers. One week ago Dugan Maddux provided us with a brief reprieve, but today it’s back to the MACRA salt mines. On the MACRA menu today is the new kid on the block; the kid formerly known as Clinical Practice Improvement Activities now has a new name—simply Improvement Activities.
The Monday after Thanksgiving. Festive celebrations with family, large meals, a bit of football, and perhaps some shopping on Black Friday are all now in the rearview mirror. It’s Monday and we are left with, well, leftovers. One week ago Dugan Maddux provided us with a brief reprieve, but today it’s back to the MACRA salt mines. On the MACRA menu today is the new kid on the block; the kid formerly known as Clinical Practice Improvement Activities now has a new name—simply Improvement Activities.
Beyond the name
Although CMS shortened the name, Improvement Activities remain an important component of MIPS. How important? Fully 15% of your MIPS score will originate from Improvement Activities. Resource Use is a no show next year, which makes this new kid the third most important MIPS category from a scoring perspective, just behind the 25% you will receive from Advancing Care Information and quite a ways behind Quality, which commands a whopping 60% of your score in 2017.
Easy button
Let’s not forget, however, that next year is a transition year. As we recently noted, those of you facing MIPS next year can simply dip your toe in the water and avoid the 4% haircut in 2019. One of the easiest ways to do that is to attest to the fact that you participated in a single Improvement Activity during an appropriate time interval next year—but more about that later.
What is an Improvement Activity?
Let’s cut to the chase. What in the world is an Improvement Activity? Wonderful question, without a clear answer. Let’s try to answer it by borrowing text from the CMS website: “In this new performance category for 2017, clinicians are rewarded for care focused on care coordination, beneficiary engagement, and patient safety.” Crystal clear, no? The final rule goes on to state that “Section 1848(q)(2)(C)(v)(III) of the Act defines an improvement activity as an activity that relevant eligible clinician organizations and other relevant stakeholders identify as improving clinical practice or care delivery, and that the Secretary determines, when effectively executed, is likely to result in improved outcomes.” Effectively CMS has pulled together a list of 92 (yes, 92) activities, which in their view will lead to improvement in the care you provide to Medicare beneficiaries. I’d list them all here but you would never make it to the end of the blog (where the enlightening part of this post resides). Instead check out this webpage, which includes the list along with a brief description of each activity.
Weighting and scoring
Not to complicate matters (this is CMS after all), but there are basically 2 flavors of Improvement Activities: those weighted heavy and those weighted medium. This is important for those of you planning to run the full MIPS gauntlet next year. The heavy-weighted activities are worth more MIPS points than the medium-weighted activities. To be more specific, the heavy weights are worth 20 points and the medium-weighted Improvement Activities are worth 10 points. Per the final rule, you need to achieve 40 Improvement Activity points in order to capture the maximum number of points available within the Improvement Activities category of MIPS. What could be simpler?
But wait, there’s more! If you find yourself in a “small practice,” which CMS defines as 15 or fewer providers, or if you practice in a rural area or a geographic HPSA (health professional shortage area), or if you are a “non-patient facing” MIPS eligible clinician (like a pathologist), you basically receive double credit for your efforts (you achieve a maximum score for a single heavy-weight or 2 medium-weight Improvement Activities). Last but not least, next year some of you will be participating in an Alternative Payment Model (like a track 1 MSSP ACO). Simply by participating in the APM, you will receive half credit for the Improvement Activity category of MIPS. Could they make this any easier?
Let’s try to summarize this mess.
- If you are part of a large group (16 or more providers) and you are not in a rural area or a HPSA, you can collect the maximum Improvement Activity category points by performing either 2 heavy-weighted Improvement Activities, 4 medium-weighted Improvement Activities, or 1 heavy-weighted and 2 medium-weighted Improvement Activities
- If you are part of a small practice (15 or fewer providers) or you work in a rural area or a HPSA, you can collect the maximum Improvement Activity category points by performing either 1 heavy-weighted Improvement Activity or 2 medium-weighted Improvement Activities
- If you are a participant in an APM, you automatically receive 20 of the possible 40 Improvement Activity points, which means you only need half of what I outlined in numbers 1 and 2 above.
All together now
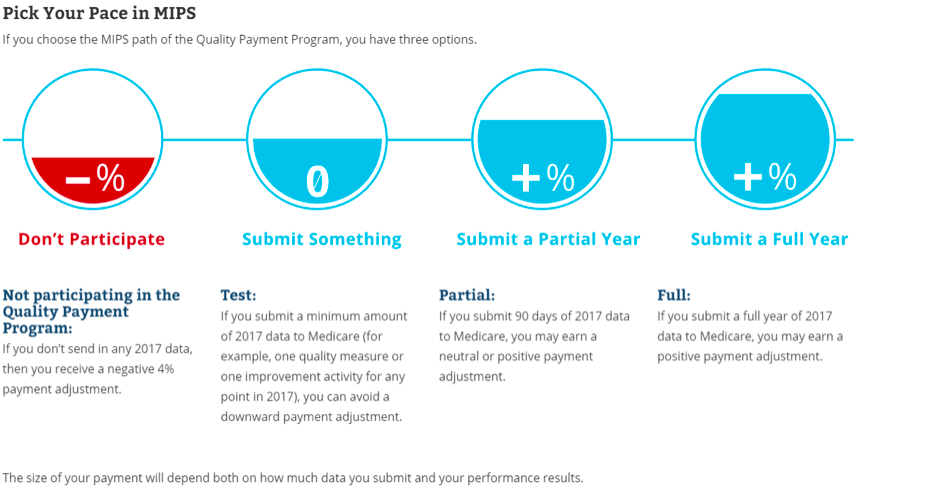
So how is this supposed to work? First determine where you find yourself in 2017 on the MIPS pick-your-pace continuum below.
As Acumen blog readers, clearly none of you are in the red circle at the far left. The Easy Button referenced above is next in line (i.e., Submit Something) and this is where I suspect many of us will land next year. Simply locate one of the 92 improvement activities on this CMS web page and put that activity in place for any continuous 90-day period during CY 2017.
If you are a bit bolder and are looking at either the Partial or Full Year circles on the right in the graphic above, remember, you are only compelled to engage in your selected improvement activities for any continuous 90-day period, even if you are participating in MIPS for the entire year.
Of course when you have finished your work here, you need to get credit for all of that improvement activity. You do this next year by attesting to the fact that you did indeed participate in said Improvement Activities for a continuous 90-day period in 2017. CMS will allow for submission of data for the Improvement Activities performance category using the qualified registry, EHR, QCDR, CMS Web Interface, and attestation data submission mechanisms. There are indeed a large number of options available to let CMS know that you’ve completed the work.
By the way, buried in the depths of this final rule is a bit of fresh air. The continuous 90-day engagement period for Improvement Activities remains in place for 2018. Seems odd to me, but there you have it. When you attest you are basically stating you’ve participated in the improvement activity for 90 straight days in 2017, and that’s apparently enough in 2018 as well.
Last but certainly not least, as you may recall from Diana Strubler’s outstanding deep dive into Advancing Care Information, there are some Improvement Activities that will count in the ACI bonus section. Unfortunately those are not clearly marked in the web page I referenced. They are however readily viewable in Table H within the final rule itself.
Pass the turkey…
As complicated as our friends at the Agency have managed to make this, the Improvement Activities category of MIPS is actually going to be one of the easiest parts of the program. My advice would be to look at the pick-your-pace graphic above and determine which circle you wish to live in next year. Then identify one or more Improvement Activities that you believe will make a difference. Pick a date next year prior to October 2, 2017, and set the wheels in motion for at least 90 days. If I were running the MIPS gauntlet next year, Improvement Activities would not keep me up at night like those Thanksgiving leftovers certainly do.
What are your thoughts about the new kid on the block? Drop us a note and join the conversation.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Top image from www.canstockphoto.com




Rg says
Wouldn’t submitting one quality measure be easier? I am referring to the submit something option, for those of us that want an insurance policy as we are in an APM.
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
My read suggests the Improvement Activity path will be easier RG. Something tells me we may hear more about the Quality side in the Acumen blog next week. Long story short, even if you are reporting Quality next year (sending in one measure to avoid the 2019 penalty), I believe for Quality you must report on the majority of the denominator eligible patients you encounter during the calendar year. Stay tuned to the blog for the details and how that may work next year. On another note, if you are in an APM, you receive half credit for the Improvement Activities category of MIPS. My read suggests that is your insurance policy if you are in an APM next year. Not sure why you would report a quality measure in addition?
rg says
Got it. But if something “goes wrong” with the APM, do we still get half credit? Should we aim for 100 percent credit in case the APM has an unexpected issue? In other news, here are some good book recs for you: Richard Thaler’s new book on the memoirs of behavioral economics, and “Making it Stick.” Both are on audible for easy listening.
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Fair point RG. One thing that could go wrong with the APM is the financials could go sideways and the participants might let CMS know they are folding their tent as it were prior to the end of the year. If that happened prior to the end of 2017, one might imagine the MIPS exclusion could vanish, and with it perhaps credit for Improvement Activities. Might depend on when during the year the APM dissolved. As easy as it looks like it’s going to be to attest to the fact that your practice initiated one of the 92 Improvement Activities, strikes me as the easy path, and if you are selective, you’ll create a bit of value beyond simply checking a box. I think each practice is going to need to make the call. Thankfully there is no hurry with ACI or Improvment Activities next year as you have the continuous 90 day reporting piece.
Anne E. Zaccheo, MBA, FACMPE says
It was my understanding from MGMA that providers in an AAPM are considered by CMS to also be a “MIPS APM” and that in 2017, all MIPS APM providers would receive full credit in the improvement activities category, not half credit? Thank you
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Excellent point Anne and thanks for clarifying. The blog should read those participating in an MIPS APM will receive At Least half credit for Improvement Activities. Apparently CMS intends to examine the criteria for each model and determine how much credit to award.The Track 1 MSSP ACO did in fact make the grade for 2017 and participants in that program (along with the Oncology Model of Care) will receive full credit for Improvement Activities in 2017. Of interest they also re weight the MIPS categories for scoring within an APM.
https://qpp.cms.gov/docs/QPP_APMs_and_Improvement_Activities.pdf
Many moving parts Anne, thanks for your comment!
Peter Manring says
Thanks for a great post Terry. We are part of a multispecialty clinic and share a common tax identification number. Some non nephrogists don’t participate in Meaningful Use or PQRS, which hasn’t affected use as > 50% of providers do. With MACRA, how will our nephrologists be identified? By NPI or tax ID number? I’m concerned our providers will look bad if mixed with non MACRA participants who share a common tax ID.
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Great question Peter. For within MIPS you have the opportunity to report as a practice at the TIN level, or individually at the NPI level. The impact of MIPS on your future fee schedule will be assessed at the NPI level based on how you’ve performed within the MIPS framework.
Tammy says
Great article! “CMS will allow for submission of data for the Improvement Activities performance category using the qualified registry, EHR, QCDR, CMS Web Interface, and attestation data submission mechanisms.” was mentioned.
Being as though an EHR has not been implemented in our practice, I can only assume we should be able to attest to our Improvement Activities via the CMS Web Interface? Is that correct? If so, would you happen to know where this interface might be found?
Thank you!
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Hi Tammy, yes you should be able to report your improvement activity via the web interface. I’d reach out to the Quality Payment Program Service Center at 1-866-288-8292 for details.