 Let’s go ahead and take a collective sigh of relief because this blog post has nothing to do with the election! Instead, I will talk about another dreaded popular topic on the regulatory front – advancing care information (ACI)!
Let’s go ahead and take a collective sigh of relief because this blog post has nothing to do with the election! Instead, I will talk about another dreaded popular topic on the regulatory front – advancing care information (ACI)!
Last week, Dr. Terry Ketchersid brought us through a vocabulary lesson on the many FLAs and TLAs of MACRA. If you don’t know what FLAs or TLAs are, then you’ll need to take a read. Not only did he spell out some of the acronyms you’ll find in the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), but he also detailed what it means to be in an Advanced Alternative Payment Model (AAPM).
For some of you, the Advanced APM track sounds very enticing. However, you may find that there are little to no opportunities in your area to even join a qualifying APM. Instead, you’ll find yourself behind the wheel of the MIPS mobile.
MU 2.0
The Merit Incentive-based Payment System (MIPS) should look somewhat familiar. Three of the 4 MIPS components are just tweaks of current regulatory programs (Meaningful Use, Physician Quality Reporting System, and the Value-based Payment Modifier).
Starting next year, the Meaningful Use (MU) program, arguably the most notorious of the 3, will not only get a name change (to advancing care information) but will receive quite the facelift as well.
Some of the most notable changes are the following:
- No longer an “all-or-nothing” program. Clinicians must report the base measures, but do not have to report all of the measures available.
- Removed the threshold requirements. Clinicians do not have to meet a certain percentage.
- Reduced the Public Health Registries requirements. Immunization reporting is no longer required but can still be selected for performance points.
- Retired 2 existing MU measures. CPOE and Clinical Decision Support will no longer be measure options.
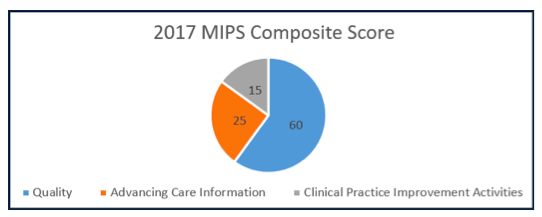
MIPS composite score
In 2017, the ACI component of MIPS will account for 25% of your MIPS composite score.
To get the full 25%, a clinician must earn the 100 points available in this category.
If you do not earn the full 100 points in ACI, you will need to do the following calculation to know how many MIPS points you will earn for this category.
(ACI performance category score x ACI performance category weight) = total ACI points in MIPS
If a clinician earned 65 points out of the total 100 ACI points, he/she would apply the following calculation:
65 x .25 = 16.5 points (out of a possible 25 ACI category points)
How to earn ACI points
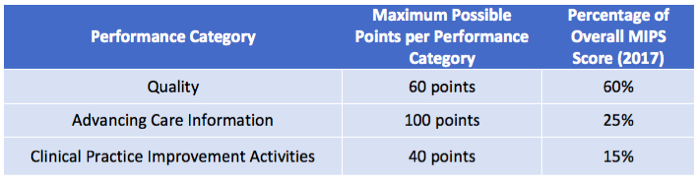
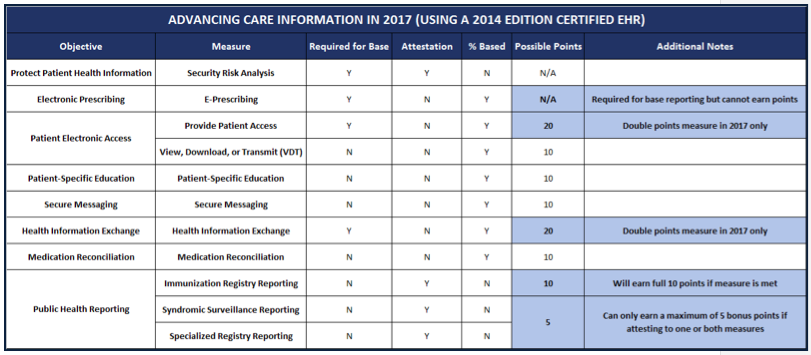
The ACI category is broken down into 3 main sections. The base score, performance score, and bonus points. Each section is allotted a total amount of possible points.
As you can see from the illustration above, getting a perfect score in each of the ACI sections could potentially earn a clinician 155 points. If a clinician earns more than 100 points, CMS will bring it back down to 100. No extra credit here!
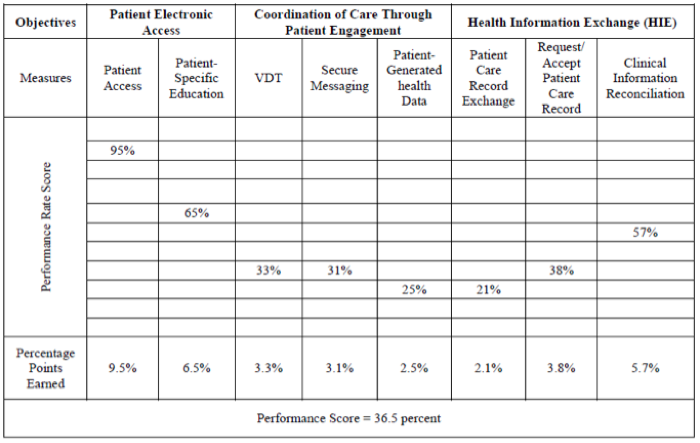
Base score
The first 50 points (aka the base score) can be earned by reporting data on the following 4 (or 5) objectives:
- Performing a Security Risk Analysis
- E-Prescribing
- Providing Patient Access to Their Data
- Sending Summary of Care via HIE
- Requesting/Accepting Summary of Care (only required in 2018 and beyond)
For each measure, you must report a yes/no for each attestation measure and at least a 1 in the numerator for each percentage-based measure.
Failure to meet the base score requirements will immediately give you a 0 in the entire ACI category!
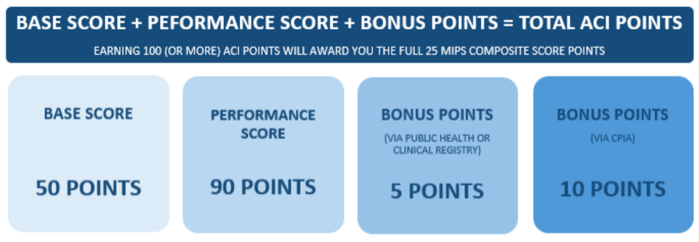
Performance score
This portion of your ACI score will be based on how well you did in measures that you choose to report. Some key words in that last sentence are “how well” and “choose.” As I mentioned earlier, CMS has taken away the concept of “all-or-nothing,” meaning a clinician doesn’t have to meet a certain threshold for every measure available. Instead, clinicians can earn the remaining 50 points by choosing which percentage-based measures he or she sees as favorable to report.
Let’s stop for a second to understand what an attestation-based measure is versus a percentage-based measure. Some of the ACI measures are considered attestation-based measures. The only possible answer for these measures is a yes or a no. You either did it or you didn’t. For example, you either did a security risk analysis or you didn’t.
As for percentage-based measures, these require a calculation of numerator/denominator. The result of this calculation will give you a performance percentage.
Each percentage-based measure is worth up to 10 points, with the exception of “Provide Patient Access” and “Health Information Exchange.” Those 2 measures are worth 20 points each in 2017.
Also, clinicians cannot report the e-prescribing measure as one of their performance measures because many clinicians already score high in this measure today.
Points earned for each measure are calculated by taking 10% of the performance score. For example, a 90% in a given measure will earn the clinician 9 points. If you are between decades (such as an 85%), you would round to the nearest whole number—in this case an 85% would be 9 points.
The immunization measure is the only performance measure that isn’t percentage based. This measure (that used to be required but now isn’t) can earn the clinician either 0 points or 10 points. There’s no in-between.
Bonus points
If you’re still struggling to get a decent ACI score, you have the opportunity to score bonus points. Bonus points can be acquired in 2 different ways:
- A clinician who reports data to a public health agency or clinical data registry can earn a maximum of 5 bonus points
- Using a certified EHR (CEHRT) to meet a clinical practice improvement activity can earn a maximum of 10 bonus points
All together now!
Here is a summary of a clinician’s ACI dashboard in 2017:
What about my certified EHR?
Now that’s a lot of details to remember. To add complexity to an already complex subject, the rules (and measures) listed above will slightly change in 2018. A few new measures will be introduced, and some will be tweaked.
In 2017, clinicians can use their current ONC 2014 edition EHR. However, starting in 2018, they will need to upgrade to an ONC 2015-edition EHR. Most EHRs are currently working towards becoming ONC 2015 certified. If yours isn’t, you may want to shop around. For those Acumen EHR customers—don’t worry, we’ve got you covered!
Due to the required upgrade, CMS is allowing for yet another 90-day reporting period in 2018 (for the ACI category only) to give clinicians enough time to make the transition.
MU improved?
Now granted, what you just read probably didn’t sound easier than the current MU program, but once you get past all of the options and math it really does lessen the load that you are carrying today. Also, keep in mind that next year is a “pick-your-pace” year. That means you can take the easy road and just report the base measures in 2017 (or at least one measure from a different MIPS category altogether).
Do you think the new “MU” got easier, harder, or is it about the same?
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Top image from www.canstockphoto.com



rg says
Where does the “fifty percent rule” fall in the new individual MIPS world? Do you anticipate the exclusion as we did previously in the M.U. program? I like the Tuesday MIPS TIPS. Very clever, whoever thought of it. Do we know yet how these measure are going to change over time? Or is the jury still out on that one?
Diana Strubler says
Hey RG! Thanks for the compliment on MIPS TIPS. I mean, with the play on words, I couldn’t pass it up!
As for your questions…
The fifty-percent rule only lives in the Advancing Care Information component of MIPS. However, beware of what this could mean. If you take the “fifty-percent rule” hardship in ACI, that means that the ACI category will be reweighted to zero and in turn your quality category will be over weighted. Currently, the quality category is worth 60%. If you take the hardship, the quality category will now be worth 85% in 2017. Now, if you are taking the easy road in 2017 (aka the “submit something” to avoid the penalty), then the hardship may not come into play this year as you only have to submit 1 quality measure OR 1 CPIA activity OR 4 base ACI measures.
The measures will change over time! I’ll tackle that in another blog post. I tried to fit it in this one but PHEW that would have been a dissertation.
Thanks for being an active blog reader/commenter RG!
Diana
Grant Wideman says
Diana,
This is the best explanation I have seen on the ACI category on the web. You really get lost trying to read it on teh CMS website. Great job.
I was wondering if you had the details of the bonus points? How are the 5 bonus points for Public Health Reporting calculated? It says everywhere “upto” 5 bonus points. At other places, it says 1 bonus point for reporting. How will the calculate the exact bonus points for this category.
thanks
Grant
Diana Strubler says
Hi Grant – isn’t this too much fun? You will automatically get the full 5 points for reporting to a public health registry. If you choose two public health registries/clinical data registries to report to – you cannot get 10 points. You will max out at 5. On top of that, some of the improvement activities (under the CPIA category of MIPS) allow you to “double dip” and also get bonus points in the ACI performance category if you use a certified EHR to meet the improvement activity. Choosing one of these activities will allow you to get a full 10 points. This opportunity is maxed out at 10 points. I hope this helps!
Diana