 Ah, the day before the election. Hard to believe that sideshow known as the Presidential race is coming to a close. As I’ve mentioned before, we tend to steer clear of religion and politics in the Acumen blog. And while it’s very tempting to break with tradition, I plan to stay on the sidelines today. Instead, let’s dive into our new favorite 4-letter acronym, AAPM (Advanced Alternative Payment Models).
Ah, the day before the election. Hard to believe that sideshow known as the Presidential race is coming to a close. As I’ve mentioned before, we tend to steer clear of religion and politics in the Acumen blog. And while it’s very tempting to break with tradition, I plan to stay on the sidelines today. Instead, let’s dive into our new favorite 4-letter acronym, AAPM (Advanced Alternative Payment Models).
The basics
We recently visited the APM topic, providing some insights gleaned from the proposed rule. The final rule reiterates and expands on what we knew before. First, let’s try to clear up some of the confusion our good friends at the agency have inadvertently created.
Starting a mere 54 days from now you will be faced with a host of new FLAs and TLAs (3-letter acronyms), each of which impact your future Medicare fee schedule. The MACRA final rule has introduced the new phrase “Quality Payment Program” or QPP, an important component in your world moving forward. Best way to think about this is the Quality Payment Program basically takes the place of PQRS, meaningful use (MU), and the physician value-based payment modifier (VPM).
Within the Quality Payment Program, you are either in an Advanced APM or you are subject to the Merit-based Incentive Payment System (MIPS). The common thread here is the work you do next year will dictate what your fee schedule looks like in 2019. This should come as no surprise to you as it is basically the same structure you’ve seen over the past 10 years with programs like PQRS, MU, and the VPM.
Most of you will face MIPS in 2017. In fact the only way to escape MIPS next year is if one of the following apply:
- You just finished your fellowship and are new to the Medicare system
- In 2017 you will either bill Medicare less than $30,000 OR have encounters with fewer than 100 Medicare beneficiaries
- You are a successful participant in an Advanced APM (like an ESCO)
For those of you not in one of these buckets, CMS has made life easier for you next year as we discussed last week.
APMs
Some of you are participating in what I’ll call regular Alternative Payment Models. The most common example is the Track 1 Medicare Shared Savings Program ACO. Today Track 1 MSSP ACOs are shared savings programs (thus the name). There is no downside risk, which is one of the things that makes them attractive to physicians. As we will see in a moment, the lack of downside risk is also the reason why they are not considered “Advanced” APMs. The upshot is this, if you are in an APM next year (like the previously mentioned Track 1 MSSP), you need to report MIPS because if you do not, CMS will apply the 4% penalty to your 2019 fee schedule.
Advanced APMs
More about “regular” APMs another day. Today we’re focusing on Advanced APMs, which include ESCOs. Advanced APMS are a special breed of APM. Per CMS, to become an Advanced APM, an APM must do 3 things:
- Require participants to use certified EHR technology
- Base payments for services on quality measures comparable to those in MIPS
- Require participants to bear more than nominal financial risk
We could spend several blog posts massaging each of the three items above. Thankfully we do not have to do so. CMS basically looks at the underlying requirements for each type of model of care, and then they decide if the APM is Advanced. For 2017, the list of Advanced APMs includes:
- ESCOs (LDO and non-LDO ESCOs that elect to take downside risk)
- MSSP ACOs (tracks 2 or 3)
- Next Gen ACOs
- Oncology Model of Care (2-sided risk arrangement)
- Comprehensive Primary Care Plus
CMS will publish the final 2017 list prior to the end of this year. The final rule also notes that additional models will become Advanced APMs in time for the 2018 reporting year. Within the final rule, CMS makes some interesting predictions. Next year they believe there will be between 70,000 and 120,000 clinicians participating in an Advanced APM. In 2018 they estimate that number will exceed 125,000 and may reach 250,000.
The “advantage” of an AAPM
Advanced APMs are attractive to docs in the short term for at least 2 reasons beyond the AAPM itself. When the providers within the Advanced APM clear defined thresholds of participation, they:
- Are exclude from MIPS, and
- Receive a lump sum payment equivalent to 5% of their entire Part B book of business from the prior year.
The first one is the biggest carrot in my view because of the cost and administrative overhead necessary to compete in the stand-alone MIPS world in the years ahead. But docs tend to discount this, so let’s be clearer about the 5% bonus. The way that works is as follows: If the AAPM you are participating in during 2017 successfully clears targets established in the final rule, permitting you to become a “Qualifying Participant,” then in 2019 you will receive a payment from CMS equal to 5% of your 2018 Part B allowable.
To these short-term advantages, CMS has added a long-term play as well. Beginning in 2026, the annual increase for your Medicare fee schedule will either be 0.25% or 0.75%. The lower number is for MIPS providers, the higher figure is for those participating in an Advanced APM.
Qualifying participant
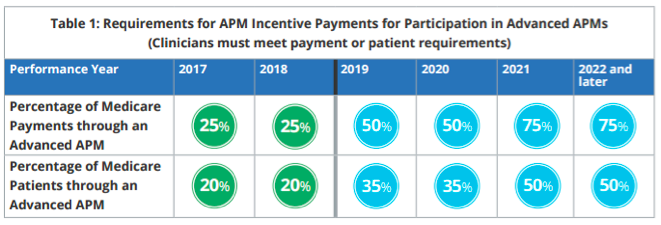
So, how do I get in line for the AAPM bounty described above? First, it probably goes without saying, but you must be a participant in one of the Advanced APMs CMS identifies each year. Second, you must meet or exceed a certain threshold for either payments or patients through an Advanced APM. Those thresholds are on display in Table 1 below:
The way to read this is as follows: I am a Qualifying Participant for performance year 2017 if one of the following 2 things occur for the Advanced APM entity I am in:
- At least 25% of the 2017 Medicare Part B payments received by participating providers come from caring for patients aligned with the Advanced APM in 2017, or
- At least 20% of the Medicare beneficiaries the participating providers care for in 2017 are aligned with the Advanced APM in 2017
Note: This is an all or none phenomena. The Qualifying Participant designation applies to every doc in the Advanced APM. It is effectively a weighted average calculation for all of the docs in the Advanced APM. If one doc in the Advanced APM receives 50% of her 2017 Part B revenue from patients in the Advanced APM, but the other docs in the Advanced APM are so far below the thresholds above that the Advanced APM entity comes in at 24% of revenue and 19% of patients, no one in the Advanced APM is a Qualifying Participant. Of course the opposite is true as well. The so called “free rider” would be a doc with very few patients in the Advanced APM, but he is designated a Qualifying Participant right along with the rest of the docs in the Advanced APM if collectively the Advanced APM achieves one of the thresholds outlined above.
The important piece of this puzzle, of course, is how do they define the denominator? The language in the MACRA final rule is lengthy, but it’s pretty clear the denominator is not your entire Medicare population, but the subset of your Medicare population who were eligible for alignment to the Advanced APM based on the APMs alignment or attribution criterion.
TLAs and FLAs
MACRA and the new Qualifying Payment Program have created a dizzying array of new acronyms for us to consume. As I noted last week, most of us will face MIPS next year. Thankfully, 2017 is a transition year with an Easy Button. The advantages highlighted above for participating in an Advanced APM are not an accident. CMS has created these financial incentives to make these models attractive to clinicians who have the opportunity to participate. It’s also very clear that over the next few years additional APMs will become AAPMs. This should provide more opportunity for nephrologists to avoid MIPS.
Over the next several weeks we will continue to unpack MACRA and the QPP. If your head is spinning and you are preparing to shout a different sort of acronym at this mess, stick with us and save those TLAs and FLAs for tomorrow’s election.
Are you participating in an Advanced APM? Drop us a note and join the conversation.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Top image from www.canstockphoto.com




rg says
I am looking ahead to 2021. How hard for it will be for the typical ESCO to achieve 75 percent or 50 percent attribution in the chart above? Does the .75 percent update occur if we join an ESCO for 3 years and then stop participating? Why do you view the individual MIPS as so difficult? Won’t the Acumen EHR do most of the work for us? Will it be harder than stage 1 M.U.? Thanks for the update, I appreciate it. My favorite opener on dialysis rounds is “Have you ever seen an election like this? What happened to the good ole days–back in my day it was Teddy R—>a decent candidate.”
William Bixby says
I just wanted to mention that the 5% bonus goes away after 2024 payment year and there will be a one year gap before the fee schedule increases occur. So just keep in mind that the 5% bonus lasts from 2019-2024.