 I can thank Dr. Ketchersid for introducing me to the works of Bob Dylan last week. I won’t say that the music is before my time, but I will say that his lyrics are definitely standing the test of time!
I can thank Dr. Ketchersid for introducing me to the works of Bob Dylan last week. I won’t say that the music is before my time, but I will say that his lyrics are definitely standing the test of time!
Had I chosen my own song from his repertoire to explain our current regulatory situation, it would be “Not Dark Yet”:
Shadows are falling and I been here all day
It’s too hot to sleep and time is running away
Feel like my soul has turned into steel
I’ve still got the scars that the sun didn’t let me heal
Perhaps a bit too disturbing? Yes, probably so.
A close second would be, “Don’t Think Twice, It’s All Right”:
I ain’t a-saying you treated me unkind
You could have done better but I don’t mind
You just kinda wasted my precious time
But don’t think twice, it’s all right
Who knew we were all so poetic here at the Acumen blog!
Well, maybe I’ll just stick to my day job. In that case, let’s continue down the 2019 proposed rule and wrap up some important changes on the MIPS side of the 2019 QPP proposed rule.
Improvement activities
You will be relieved to hear that the changes proposed for the other 3 categories of MIPS are not as dramatic as Promoting Interoperability (which warranted its own blog post).
For improvement activities (IA), the only thing changing is the inventory of activities available—some will be added, modified, and removed. Clinicians will only need to report on this category for a 90-day reporting period.
A disappointing change is the proposed removal of the IA bonus which allowed clinicians to receive 10 bonus points under the “Promoting Interoperability” category if they selected certain IA measures.
Otherwise, it is business as usual.
Cost
The biggest change in this category is the weight assigned in year 3. We were all anticipating that cost would rise to a whopping 30% of your overall MIPS score in 2019, but CMS suggests dialing it down to 15%. Phew. They also propose adding additional flexibility to the weighting of this category for three additional years, requiring the weight to be no less than 10 percent and no more than 30 percent for the third, fourth, and fifth years of the QPP.
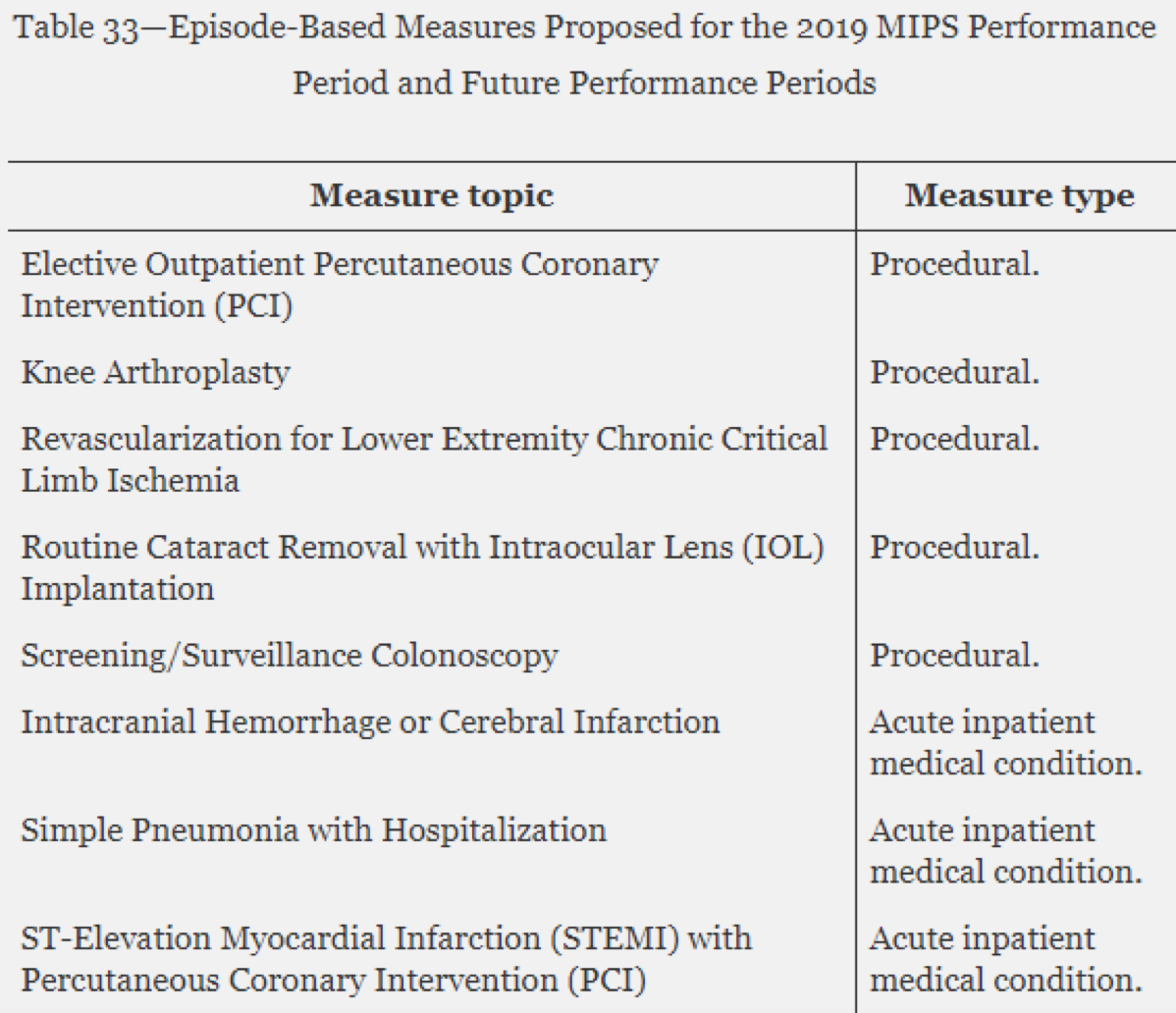
The other notable change in this category is the addition of 8 episode-based measures. This will be on top of the 2 measures out there today: Medicare Spending Per Beneficiary (MSPB) and Total Per Capita Cost (TPCC).
Episode-based measures differ from the MSPB and TPCC measures because the measure specifications only include items and services that are related to the episode of care for a clinical condition or procedure, as opposed to including all services that are provided to a patient over a given timeframe. More on this one later!
The 8 measures proposed are listed below. If you really want to know the details of each one, take a peek at the measure specification drafts.
Lastly, CMS also proposes removing the improvement scoring bonus points in 2019 and beyond.
Quality
As complicated of a category as quality is, the changes for 2019 are rather small.
The overall weight will go down to 45% (due to the cost weight going up). The other rules for selecting and submitting measures stays the same.
New to the ruling is the way CMS proposes handling quality measures that get updated during the performance period. Updates to clinical guidelines for a measure can happen outside the rulemaking cycle. In some instances, a measure change can significantly impact the way the measure is calculated, and not following the new measure change could put the patient at risk.
In these cases, if a measure change is significant (or could cause a patient safety issue), CMS will let clinicians know and modify the quality category scoring. For clinicians who selected that measure, CMS proposes reducing their quality category total points possible by 10 points so it would not negatively impact their performance.
CMS proposes yet another change to bonus points—moving the small practice bonus from the final score level to the quality-performance score level. This change will significantly reduce the impact of these 3 points.
Payment adjustments
The last topic we’ll cover is the change in how CMS will apply your payment adjustment.
For those of you who may receive a bonus (or incur a penalty), CMS proposes to change the application of MIPS payment adjustments.
The Bipartisan Budget Act of 2018 provides that any MIPS adjustment factor will apply only to Part B payments for covered professional services furnished by the MIPS-eligible clinician during the year. The adjustment factors will not apply to all items and services under Medicare Part B (such as drugs).
But there’s more!
I anticipate that Dr. Ketchersid will wrap us up on the APM side of the 2019 QPP ruling in the coming weeks. If you are chomping at the bit to learn more now, I would suggest listening to the webinar CMS hosted recently or glancing through their slide deck.
As a reminder, everything we covered in the past few weeks is still in a proposed state. If you want to have your voice heard, you can write to CMS by September 10. Instructions on how to submit comments can be found at the top of the proposed rule.
Do the proposed changes get us closer to a better “triple AIM” solution? Or is this another confusing change to the game?
The answer my friend, is blowing in the wind, the answer is blowing in the wind.
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Image from www.canstockphoto.com




Leave a Reply