 The first week of November was a busy one for the Centers for Medicare and Medicaid Services (CMS). Not only did they release the 2019 Physician Fee Schedule (PFS) but also the 2019 Quality Payment Program. According to CMS, the monumental changes made will address provider burnout by “shifting clinicians’ time from completing unnecessary paperwork to providing innovative, high-quality patient care.”
The first week of November was a busy one for the Centers for Medicare and Medicaid Services (CMS). Not only did they release the 2019 Physician Fee Schedule (PFS) but also the 2019 Quality Payment Program. According to CMS, the monumental changes made will address provider burnout by “shifting clinicians’ time from completing unnecessary paperwork to providing innovative, high-quality patient care.”
Let me preface by saying that this is one of many blogs to come! There is so much to unpack between the PFS and QPP, therefore we will need to take it in digestible chunks. We will start with a high-level overview of the QPP final rule.
Overall 2019 MIPS program changes
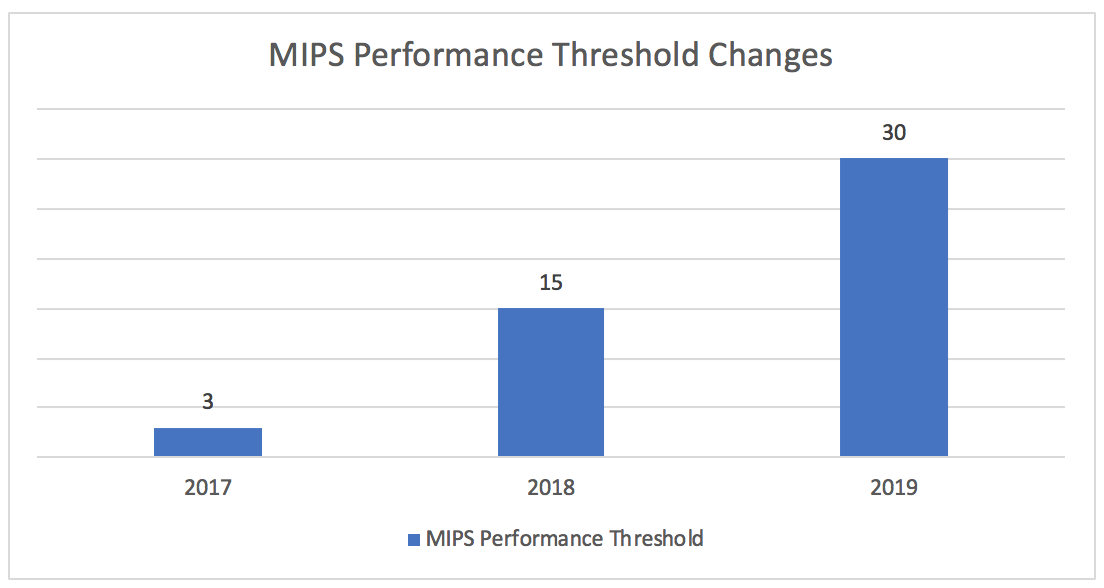
Performance Threshold
The magic number this year to avoid a negative payment adjustment is 30. This is double the threshold from last year—but still a relatively low bar. For those wanting their shot at part of the $500M exceptional performance bonus pool, you must score at least 75 points (up 5 points from last year). To put things in perspective, the average score in 2017 was 55.08 and only 5% of eligible clinicians received a negative payment adjustment.
Money
For those who earn anywhere between 0 to <30 points, the maximum negative payment adjustment is set at -7% for the 2021 payment year. For those who earn >30 points, the payment adjustment can be up to 7% (but the upward payment adjustment factor is multiplied by a scaling factor to achieve budget neutrality, which could result in an adjustment above or below 7%). Given that last year’s perfect scorers only earned up to +1.88%, it is doubtful with the lower bar set this year that anyone will meet or exceed a +7% bonus. CMS estimates there will be 798,000 eligible clinicians at play next year and approximately $390M in payment adjustments will be redistributed (not including the $500M exceptional performance bonus pool).
Expanding Clinician Types
The eligible clinician definition expands to include the following clinician types in year 3:
- Physical Therapists
- Occupational Therapists
- Qualified Speech-language Pathologists
- Qualified Audiologists
- Clinical psychologists
- Registered dietitians or nutrition professionals
Low-Volume Threshold
The low-volume threshold now includes a third criterion for determining MIPS eligibility. To be excluded from MIPS, clinicians or groups need to meet one or more of the following 3 criterion:
- Have ≤$90K in Part B allowed charges for covered professional services
- Provide care to ≤200 Part B enrolled beneficiaries
- (NEW!) Provide ≤200 covered professional services under the Physician Fee Schedule (PFS)
Also new to year 3 is the ability to opt-in to MIPS even if you meet at least one (but not all three) low-volume threshold criteria.
Reweighting
A weight of 0% will be assigned to all 4 performance categories (and a neutral payment adjustment will be applied) for clinicians in the following circumstances:
- A MIPS eligible clinician joins an existing practice (existing TIN) in the final 3 months of the performance period year and the practice is not participating in MIPS as a group
- A MIPS eligible clinician joins a practice that is a newly formed TIN in the final 3 months of the performance period year
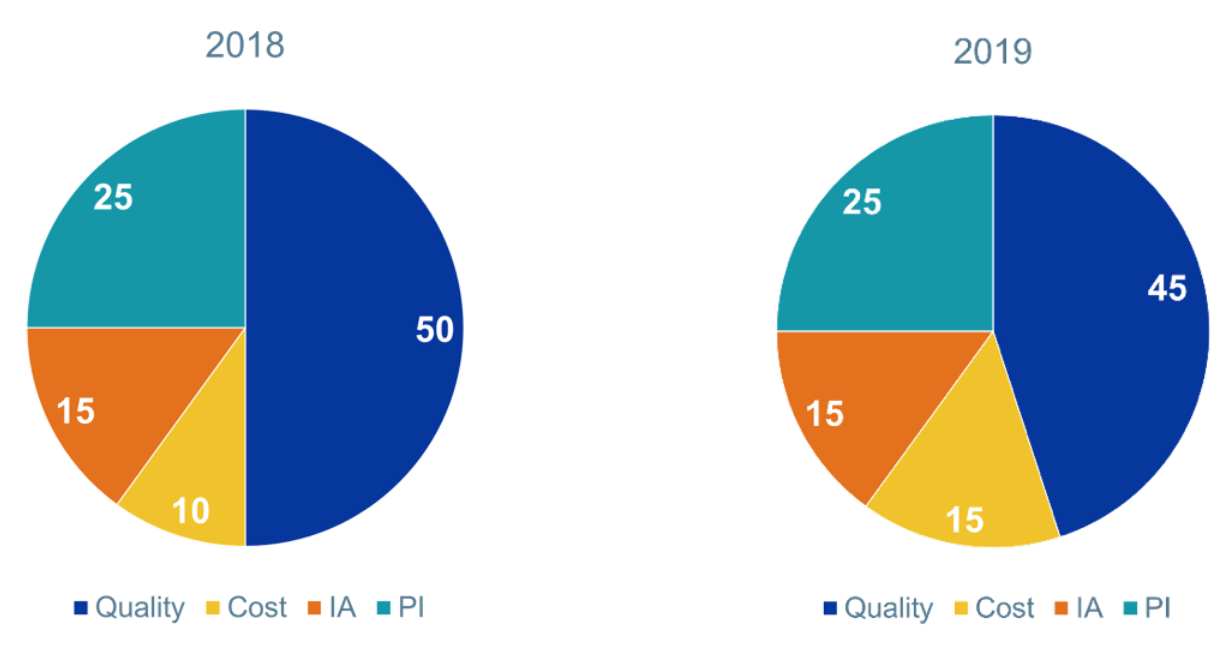
MIPS Category Weights
The category weights haven’t changed much between years 2 and 3. The cost category bumped up to 15%, while the quality category went down to 45%. This is a big relief from CMS’s original thoughts on bumping cost up to 30% in year 3.
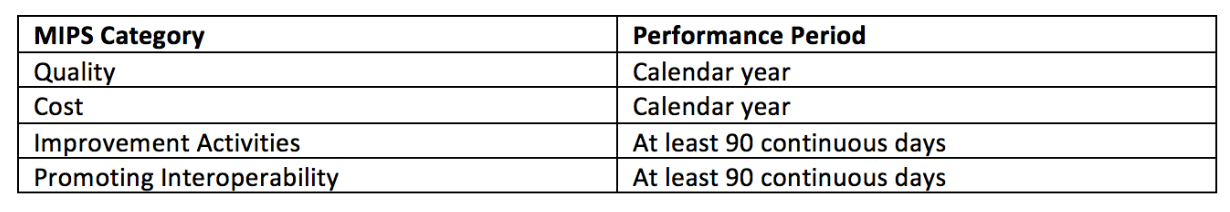
Performance Period
The performance period for year 3 has not changed. The improvement activities and promoting interoperability categories of MIPS still allow for a minimum of 90 continuous days.
Bonuses
- Small practice bonus: This bonus is now worth 6 points (up 1 point from this year) and will now be added to the quality performance category rather than the final MIPS score. This shift makes the bonus points less impactful
- CMS will retain the 5-point bonus added to the MIPS Final Score for clinicians who treat medically complex patients
Public Reporting on Physician Compare
MIPS category performance information will be available for public reporting on the Physician Compare website and associated downloadable databases.
- Quality: All measures are available for public reporting. CMS will not publicly report first-year quality measures for the first 2 years a measure is in use
- Cost: Subset of cost measures is available for public reporting. CMS will not publicly report first-year cost measures for the first 2 years a measure is in use
- Promoting Interoperability: Includes a “successful” performance indicator for eligible clinicians or groups
- Improvement Activities: For those eligible clinicians and groups that successfully
meet the improvement activities performance category requirements, this information will be posted on Physician Compare as an indicator
MIPS performance category changes
We will take a much deeper dive into the specific category changes in future blog posts, but here are some quick cliff notes:
Quality
- Category weight: 45%
- Claims-based measures can only be submitted by clinicians in a small practice (15 or fewer eligible clinicians)
- Eligible clinicians or groups can mix and match their collection types. For example, some measures can be sent via EHR and others via QCDR. If the same measure is submitted via multiple collection types, the measure that scores highest will prevail
- Groups who report 5 or fewer quality measures and do not meet the CAHPS for MIPS sampling requirements, will have their quality denominator reduced by 10 and the missing measure will receive zero points
- (NEW!): Extremely topped-out measures (a measure with an average mean performance between the 98th to 100th percentile range) will be proposed for removal in the next rule-making lifecycle. QCDR measures are excluded from the topped-out measure life cycle
Cost
- Category weight: 15%
- The Total Per Capita Cost (TPCC) and Medicare Spending Per Beneficiary (MSPB) measures remain the same in Year 3
- CMS will also add 8 new episode-based measures to the Cost performance category
Promoting Interoperability
Of all the categories under MIPS, PI was hit the hardest. I covered the proposed changes to this category back in a July blog post. Most of the proposed changes made it to the final rule.
- Category Weight: 25%
- Removed the 2015 Edition CEHRT bonus. Eligible clinicians will be required to use a 2015 Edition CEHRT in year 3
- Elimated the “base, performance, and bonus score” structure. Instead, clinicians are required to report certain measures from each of the four objectives, unless an exclusion is claimed
- Added 2 optional measures: Opioid Treatment Agreement and Query of PDMP
2019 Promoting Interoperability Measures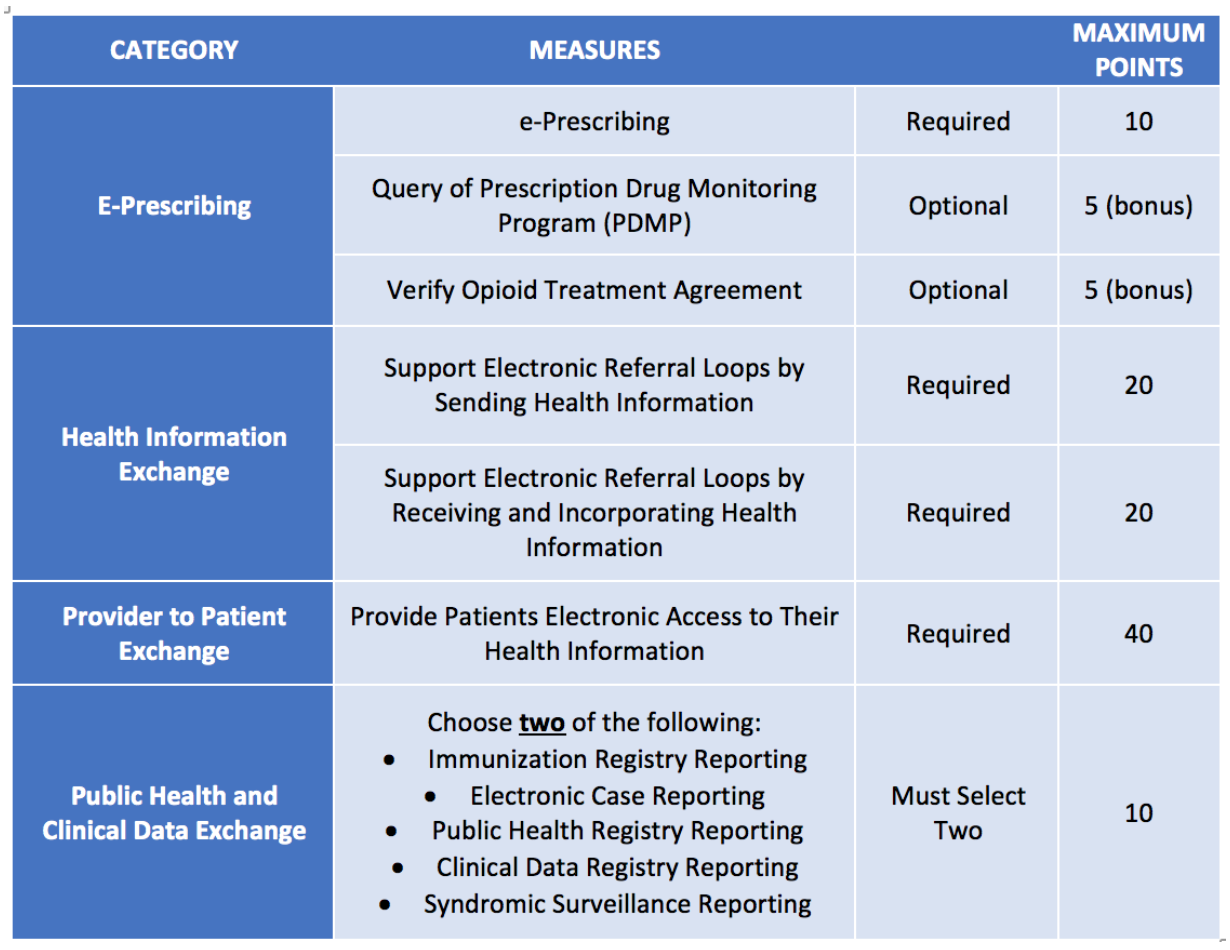
Improvement Activities
- Category weight: 15%
- Removed the improvement activities bonus that allowed 10 points to be added to the PI category if a clinician completed certain improvement activities using a CEHRT
- Added 6 new activities, modified 5 existing activities, and removed 1 existing activity
Additional Resources
We just scratched the surface of the 2019 QPP final rule, but we have to stop somewhere to avoid nausea! If you can’t wait for our future blog posts, there are other resources that CMS has published to help you digest the large rule.
- Year 3 final rule overview fact sheet
- Year 3 final rule executive summary
- Final policies for Year 3 of the Quality Payment Program (Federal Register)
- A quick start guide to the Merit-Based Incentive Payment System (MIPS) for 2019 participation
How do you feel about the 2019 MIPS changes? We’d love to hear your thoughts below!
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Image from www.canstockphoto.com



Leave a Reply