Recently in this blog Terry pointed out that the Emperor may, in fact, not be wearing new clothes when it comes to the impact of the value-based payment modifier (VM). At the risk of turning value into the worrisome pea in The Princess and the Pea, today we’ll talk about how and why value-based payment is coming.
A little background
The July 14th blog post referred to JASON, a group of scientists convened to provide council to the government on science and technology issues, who produced the report, “A Robust Health Data Infrastructure,” for the Agency for Healthcare Research and Quality (AHRQ). The White House, specifically the President, has assembled a similar group, the President’s Council of Advisors on Science and Technology (PCAST). In May, PCAST released a report to the President, “Better Health Care and Lower Costs: Accelerating Improvement through Systems Engineering,” which provides a broad overview of health care reformation. The recommended system overhaul begins with health care payment reform and data utilization to open the way for a systems engineering approach to revitalization of U.S health care.
Systems engineering for health care
So, you’ve been to medical school and you’ve never heard of systems engineering? No wonder, since this is the bread and butter of the manufacturing and aviation industries. As described in the PCAST report, system engineering “…is an interdisciplinary approach to analyze, design, manage, and measure a complex system in order to improve its efficiency, reliability, productivity, quality, and safety.” The systems engineering approach is designed to achieve high reliability with maximum efficiency, which should sound familiar: high-value health care at low cost.
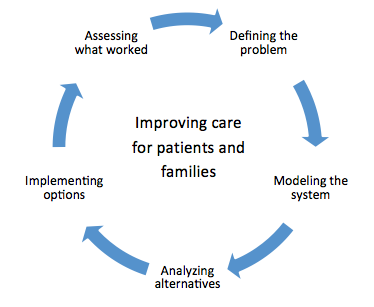
Here is the systems-engineering process PCAST envisions for health care:
How is this systems-engineering approach related to the value-based payment modifier? That story begins on page 14 of the PCAST report. The current health care environment has some major impediments to systems-engineering improvements including, “lack of quality and performance measures and the misaligned incentive structure of the predominant fee-for-service payment systems, which encourages a fragmented delivery system.” The report outlines 6 “overarching goals” for the President and administration to adopt:
- Accelerate alignment of payment systems with desired outcomes
- Increase access to relevant health data and analytics
- Provide technical assistance in systems-engineering approaches
- Involve communities in improving health-care delivery
- Share lessons learned from successful improvement efforts
- Train health professionals in new skills and approaches
What does this mean for us?
It is clear from these goals that the health care payment system must and will change as step one in improving the U.S health care system. We can’t get to the other improvements in care without this change from payment for volume to payment for value. Payment for value will require the development of valid and meaningful patient and population outcome measures.
Outcome measures are different from the process-of-care measures we have today. Outcomes measures must be meaningful for patients; they must be “measures that matter.” In addition, payers must agree to an accepted group of outcomes measures, so that providers are not trying to meet a plethora of measures in order to receive payment. These outcomes-based quality measures should be visible to support ongoing improvement in care.
The PCAST report provides specific recommendations for the alignment of payment systems with quality outcomes:
1.1: Health and Human Services (HHS) should convene public and private payers (including Medicare, Medicaid, State programs, and commercial insurers) and employers to discuss how to accelerate the transition to outcomes-based payments, promote transparency, and provide tools and supports for practice transformation. This work could build on current alignment and measurement improvement efforts at the Center for Medicare and Medicaid Services (CMS) and HHS broadly.
1.2: CMS should collaborate with the Agency for Healthcare Research and Quality (AHRQ) to develop the best measures (including outcomes) for patients and populations that can be readily assessed using current and future digital data sources. Such measures would create more meaningful information for providers and for patients.
This is a good story for providers. We can help to design and validate “measures that matter,” using data collected in EHRs and clinical systems. We can benefit from the requirement that all payers accept valid value measures and pay for them. We can participate in this realignment of incentives to focus on desired patient outcomes.
When there’s obviously an out-of-place pea in the system, such as an invalid value-based payment measure, who better than the patient-care providers to point out that it must be removed? As Hans Christian Andersen says, “There, that’s a true story.”



Leave a Reply