 I have written so many times about the eRx penalty that many of you must be tired of hearing about it. If that’s the case, stop reading now and come back next week! Of course I am kidding as I have come across some new information this week that I want to share with you. But first a little background:
I have written so many times about the eRx penalty that many of you must be tired of hearing about it. If that’s the case, stop reading now and come back next week! Of course I am kidding as I have come across some new information this week that I want to share with you. But first a little background:
2012
This is the first year nephrologists and other eligible professionals have faced a penalty from one of the CMS “big three” (eRx, PQRS, and Meaningful Use). Many nephrologists were shocked to learn they are receiving 99% of the Medicare Part B Physician Fee Schedule (PFS) for their entire Part B book of business this year. One percent sounds like a small number, but based on the reported 2010 results, it is approximately $3,200 for the average nephrologist. From a financial perspective this penalty hits the doc where it hurts—it comes right off the practice’s bottom line.
How do you know if you are taking the hit this year? A couple of months ago I discussed how you could navigate the quagmire and determine if you are indeed being penalized this year. Those of you who feel you are being inappropriately penalized should call the Quality Net Help Desk and make your case.
2013
As most are aware, the penalty increases to 1.5% in 2013. That’s roughly $4,800 based on the averages we saw in 2010 for nephrologists. The tragedy in this mess is that it is actually very easy to avoid the penalty (assuming someone in the middle does not drop the ball—more about that later). I have written about avoiding the penalty before and this brief PDF from CMS does a fantastic job of covering the topic. What I want to call to your attention is the following:
If you report the eRx G-code (G8553) for 10 Medicare PFS encounters during the first 6 months of this year, you will avoid the penalty. Note they will count this G code on any encounter. This is different from last year when the encounters all had to be incentive eligible (typically office encounters for nephrologists). For example, if I send a script electronically for a Part B dialysis patient while I am making rounds, I can add the G-code to the claim I submit for that month’s MCP charge. If I discharge a Medicare Part B patient from the hospital and send a discharge script electronically, I can add the G-code the claim I submit for that hospital charge.
One of our readers recently sent me an email stating they were receiving conflicting stories from CMS (what a shock). They were suggesting the G-code could be put on the claim, even if the prescription was generated and transmitted outside the context of the encounter (e.g. Part B patient calls in for a renewal, the doc sends the script electronically, patient comes in a month later for something else and the G-code is put on that claim). I have not been able to independently confirm this, but if you have information to share along these lines, comment below so we can share with the community. My concern with this line of thought is the description for G8553 which states the script was created during the encounter.
Potholes to avoid
Some of us learned some valuable lessons last year related to the magical mystery ride your claim takes between leaving your office and arriving at CMS. Unlike this example displayed on the CMS website, most providers are adding a charge of $.01 next to the G-code to prevent the code from mysteriously disappearing before it gets to CMS. The beneficiaries are not charged the penny, but some clearinghouses apparently have a nasty habit of deleting codes that are not accompanied by a charge. This practice should also be considered by those of you still submitting G-codes on claims as part of claims-based PQRS reporting. Registry reporting, on the other hand, is quite a bit easier.
One other pothole to consider: I heard from a reader last week that their practice management system discovered that their recent transition to the 5010 transaction standards had nixed every G-code they have submitted this year. Her practice uses an otherwise very reliable PM vendor. I would suggest picking up the phone and calling yours today to make sure you are not in the same boat.
Penalties are no fun and I do not relish writing about them, but we owe it to our colleagues to spread the word. Two months is plenty of time to avoid this penalty. Put that G-code on the appropriate claims between now and June 30, and do what you can to ensure it makes the journey all the way to CMS.

RG says
Question 1: I think you said something in one of your other posts that states if we qualify for M.U. (in 2011), we do not have to worry about this penalty. Are there any other updates on this topic?
Comment 2: A doc at our hospital uses the same PM vendor as us, but for some reason they are being penalized, but we are not. They don’t use acumen but use another EMR (same company as the vendor PM). I thought this was odd, and I referred them to the hardship exemption you pointed out to us.
Comment 3: Even if #1 above comes to fruition, it is probably best to put in 25 claims per provider as an insurance policy.
Comment 4: Can we do a registry based approach and the claims based approach, as an insurance policy? Or, is that over-kill, and will the CMS system recognize a redundant method of reporting.
Comment 5: Regarding the medicaid version of MU, the state of VA has not given us any updates on how to do this. It is appealing for obvious reasons, and I think many nephrologists would qualify since many of us have more than 30 percent medicaid patients. Stay tuned.
Terry Ketchersid, Vice President and Medical Officer at HITSG says
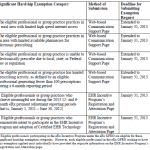
Unlike last year, the hardship exemption for participating in meaningful use will not be available in 2012. Provider’s who are successful meaningful users in 2012 must still meet one of the eRx adjustment period criteria in order to avoid the eRx penalty (being a meaningful user of a certified EHR in 2012 will not be enough to avoid the penalty). Regarding registry and claims based reporting of eRx, you can submit both but CMS will not mix and match (reporting 10 scripts via registry and 15 via claims will not suffice). Also remember successful registry reporitng of eRx in 2012 will avoid the 2014 penalty. The only remaining way to avoid the 2013 penalty is claims reporting during the first 6 months of 2012.