 I know it is difficult to believe but February is rapidly drawing to a close. Those of you keeping track of the Chinese zodiac are keenly aware that we are now one week into the year of the snake. From a CMS incentive program perspective, however, one could consider 2013 the year of the penalty. This year is the payment adjustment reporting period for PQRS and for Meaningful Use in 2015. The first half of 2013 is also one of the payment adjusting reporting periods for the last year of eRx (2014). Year of the snake it is, but year of the penalty seems more apropos.
I know it is difficult to believe but February is rapidly drawing to a close. Those of you keeping track of the Chinese zodiac are keenly aware that we are now one week into the year of the snake. From a CMS incentive program perspective, however, one could consider 2013 the year of the penalty. This year is the payment adjustment reporting period for PQRS and for Meaningful Use in 2015. The first half of 2013 is also one of the payment adjusting reporting periods for the last year of eRx (2014). Year of the snake it is, but year of the penalty seems more apropos.
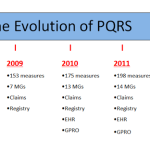
Internally we are closing out another successful year of the Acumen PQRS Registry. As we finish up our fourth year of Registry reporting, it is time to turn our attention to what PQRS 2013 has in store.
Let’s start with a clear understanding of the phrase “payment adjustment reporting period”. From the perspective of PQRS, CMS is surveying provider behavior in 2013 in order to determine whom to levy a penalty upon in 2015. In other words, the action you take this year will determine whether or not you will face a 1.5% reduction in your entire Medicare Part B book of business in 2015. The dollar amount will vary by provider, but based on published information from 2010, this could represent about $5,000 for the typical nephrologist. Today let’s focus on what you can do this year to avoid a PQRS haircut in 2015.
According to the 2013 PFS final rule there are basically three ways an eligible provider can avoid the looming penalty:
- Successfully report PQRS in 2013 (which will also generate a 0.5% bonus on the provider’s 2013 Part B book of business).
- Report one individual measure or one measures group for at least one patient in 2013 (you will be excluded from the penalty simply by making an effort to report).
- Elect to participate in the “administrative claims” reporting mechanism in 2013.
If this sounds familiar, you have been paying attention to these programs. CMS is using an approach that resembles their approach to the eRx penalty:
- Option 1—You avoid the 2015 penalty if you successfully participate in the PQRS program this year.
- Option 2—You can easily avoid the penalty if you do not fully participate (recall how easy it is/was to avoid the eRx penalty compared with full participation).
Missing from the list is participating in meaningful use. Look for that option next year when the Stage 2 CQMs make it easier to align PQRS and meaningful use.
The new kid on the block is Option 3. Basically CMS is creating a mechanism whereby the provider can actively opt into a program in which CMS analyzes your claims and specifically looks for Medicare beneficiaries eligible for 17 measures. As stated in the final rule:
“Unlike the traditional PQRS claims-based reporting mechanism, the administrative claims-based reporting mechanism we proposed does not require an eligible professional to submit quality data codes (QDCs) on Medicare Part B claims (77 FR 44825). Rather, using the administrative claims-based reporting mechanism only requires that an eligible professional or group practice submit Medicare claims to CMS. Since CMS, rather than the eligible professional or group practice, is performing the analysis and collecting the data provided in an eligible professional’s or group practice’s Medicare claims for an eligible professional’s or group practice’s Medicare beneficiaries, we believe it is appropriate to propose a reporting threshold that is more stringent than that proposed for the 2013 and 2014 incentives that use traditional PQRS reporting mechanisms. Therefore, we proposed the following criteria for satisfactory reporting for the 12-month reporting periods for the 2015 and 2016 payment adjustments (that occur in 2013 and 2014 respectively) for eligible professionals and group practices using the administrative claims-based reporting mechanism: Report ALL measures in Table 63 of the proposed rule for 100 percent of the cases in which the measures apply. The administrative claims option is temporary and only applies to the 2015 payment adjustment period (2013).”
Bottom line, if you are not interested in actively participating, you may register for this election before October 15, 2013 and CMS will not penalize you in 2015. Later in the final rule they decided to limit this option to 2013 for 2015. I must say this one makes me a little nervous and it would indeed be my third choice.
The year of the snake is underway and we find ourselves surrounded by penalties. Positive incentives still exist although they are declining somewhat in value. On the bright side, CMS is making it much easier to participate in PQRS via Registry reporting in 2013. I will review the new and improved reporting method for the CKD measures group in a future post.


RG says
Terry,
We are not putting the “G code” on claims when we do an E-Rx. I just want to clarify that if we participate in PQRS we get “credit” for the E-RX (option 1 above). That sounds like we get credit for one program while participating in another. Also, I thought I remember reading somewhere that if we complete meaningful use, we get credit for the E-RX. If this is true, what is the reasoning that CMS has whereby if you participate in PQRS you are a successful e-prescriber. Thanks, RG
Terry Ketchersid, Vice President and Medical Officer at HITSG says
Randy,
The PQRS and the eRx programs are not related. I am simply pointing out the similarities between the mechanisms to avoid the penalty in both programs. CMS is using the same pattern, if you will, for PQRS which they used for eRx.
You are correct regarding meaningful use and the eRx penalty. If you demonstatred MU during one of the 2014 payment adjustment reporting periods, CMS has stated you will not be penalized for eRx. So for example, if you demonstated MU during CY 2012 (one of the 2014 eRx payment adjustment reporitng periods) you should receive credit for eRx and not face the 2014 eRx penalty.
Having said that, it does not hurt to still put the eRx G-code on 10 Part B claims submitted for service that involved an electronic prescription….think of it as insurance against the 2014 penalty.