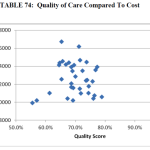
Last week I mentioned the arrival of the much-anticipated 2013 PFS final rule. Beyond the very important PFS, nephrologists will be interested in the Physician VBP. As you may recall, the VBP is part of CMS’ drive to transform itself from a passive payer to an active purchaser of quality health care. In a nutshell, the VBP is an effort to reward high-quality care delivered at low cost by penalizing low-quality care delivered at high cost. In other words, this is a budget neutral program.
A quick glance at the details
Like most of these programs, understanding the detail is where the rubber meets the road. Explaining the detail for this program would almost require writing a novelette. If I might paraphrase, CMS intends to measure physician performance by “mashing up” four levels:
- The individual provider’s performance
- The group practice’s performance
- The local facility’s performance (e.g., hospital)
- The local medical community’s performance (e.g., local health system medical staff)
Using remarkably detailed methods, at least the first three levels will be combined in the first wave of the program and then risk stratified to provide the numerator in the health care value equation:
Value = Quality/Cost
The denominator will use claims-based data to assign costs, which will also be risk stratified. Patient attribution will involve another view of claims data. Suffice it to say, this is a new ballgame for physicians and one in which very few of us have experience.
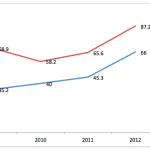
Good news for nephrology, for now
The final rule raised by a factor of four the size of practices that will be exposed to the VBP during the first wave. Those of you who practice in groups of less than 100 providers can breathe a sigh of relief. Providers by the way, are broadly defined in section 1848(k)(3)(B) of the Social Security Act to include basically every man, woman and child (okay, perhaps the kids are not counted) registered in PECOS. The program will examine provider behavior in groups of 100 or more during 2013 and 2014. A large portion of the quality piece of the equation will originate from the PQRS program. The 2013 “surveillance” period will impact payment in 2015 for these large practices, with behavior in 2014 driving the program in 2016.
The “small groups” of less than 100 providers in which most nephrologists find themselves in can sit on the sidelines and watch as this program unfolds over the next two years. As written today, all providers will face the program in 2017, which in effect means everyone’s performance data will be under scrutiny in 2015. Note that if you elect not to participate in PQRS during these adjustment-reporting periods, you will incur not only the PQRS penalty, but will be subject to a non-participation VBP penalty as well.
This program is not receiving a lot of airtime, but I believe it is an important example of a fundamental shift underway in health care today. In effect, the VBP is the physician equivalent of the QIP that dialysis programs face and the hospital value-based purchasing program that focuses on readmission rates. Ignoring this shift will not make these programs go away. Instead I would suggest you begin paying close attention to the performance measures you report to CMS, like PQRS and the CQM component of meaningful use. Participate early and gain as much experience as possible. 2015 will be here before you know it.
[…] program. Make no mistake about it, however; ESCOs will likely join the rapidly approaching Physician Value-Based Payment Modifier as forces that shift focus away from business as usual in the day-to-day lives of […]