 Can you believe we are starting the second full week of December? Not that I am counting, but I heard there are 12 shopping days left ahead of that big holiday on the horizon. Which, of course, means 2017 will soon be in the rear mirror. My how time flies when you are having fun! Speaking of having fun, I am reminded of when I started writing this blog. Seven years ago a couple of my colleagues within the Acumen leadership team persuaded, cajoled, lured (you get the point) me into writing a blog. I thought it was a crazy idea. What would I write about? Who would read it? Why would they read it? I was finally convinced to say “yes”, thinking it would only last a few months. From the beginning I established some ground rules and the most important one was “never discuss religion or politics.” Today I intend to bend that rule, as we are going to bump up against the politics boundary, but we will do so for the very best of reasons: our PATIENTS.
Can you believe we are starting the second full week of December? Not that I am counting, but I heard there are 12 shopping days left ahead of that big holiday on the horizon. Which, of course, means 2017 will soon be in the rear mirror. My how time flies when you are having fun! Speaking of having fun, I am reminded of when I started writing this blog. Seven years ago a couple of my colleagues within the Acumen leadership team persuaded, cajoled, lured (you get the point) me into writing a blog. I thought it was a crazy idea. What would I write about? Who would read it? Why would they read it? I was finally convinced to say “yes”, thinking it would only last a few months. From the beginning I established some ground rules and the most important one was “never discuss religion or politics.” Today I intend to bend that rule, as we are going to bump up against the politics boundary, but we will do so for the very best of reasons: our PATIENTS.
A bit of history
For the past few years, I have been deeply embedded within our Integrated Care Group. I have had the privilege to work with, and learn from, some very remarkable individuals. I have also had a ring-side seat as the payment models for caring for patients with ESRD have evolved from the fee-for-service world we all grew up with, to the substantially less flawed models that constitute the value-based care arena. Humor me for a few minutes as we take a walk down memory lane.
The “demo”
Over 10 years ago, three organizations participated in a five-year CMS demonstration project tasked with determining whether or not coordinating care for ESRD patients would improve quality and lower costs. Our participation in this demonstration led us to believe the answer to that question was an unequivocal “yes”. Although in retrospect the interventions delivered during that demo now appear rudimentary, we were able to demonstrate improvements in the value of the care delivered to the Medicare beneficiaries we cared for in the program.
Medicare Advantage CSNP
Another key step in this evolutionary path was the emergence of ESRD as a recognized chronic condition within the Medicare Advantage Chronic Special Needs Plan (C-SNP) program. Imagine that, payers can create a Medicare Advantage plan designed specifically for patients with ESRD. During our experience with the MA C-SNP world, we have learned a number of things about what patients want, and importantly what they need from a payer. The biggest challenge with the CSNP model? The payer is compelled to play in the general Medicare Advantage world, where the expectation is that one has thousands of patients, the majority of whom are reasonably healthy, permitting them to subsidize the care of those less fortunate. That’s not the case in a plan where all members have ESRD, which makes scale remarkably important.
The ESCO
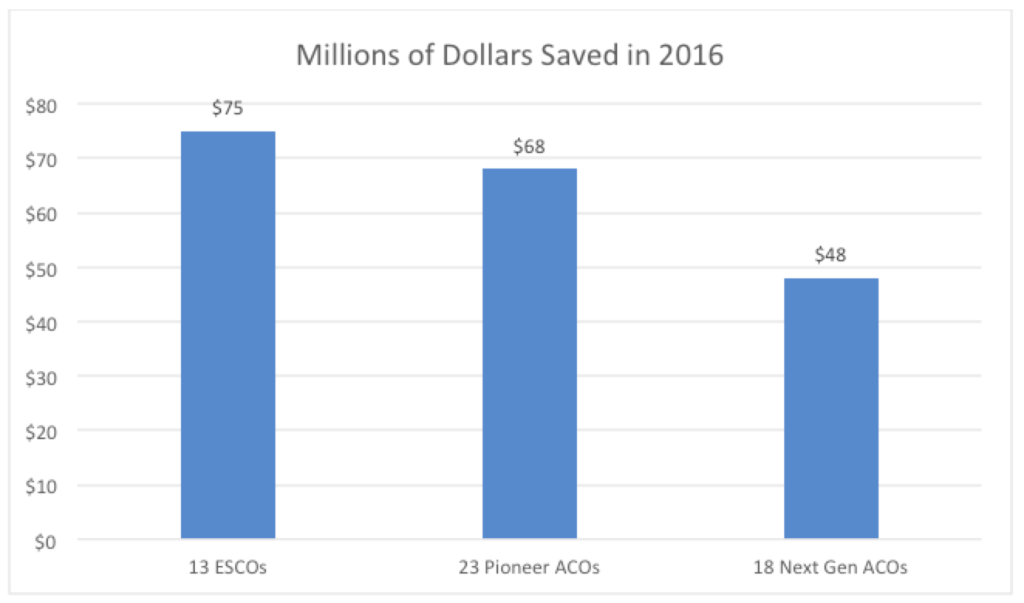
Two years ago we jumped in bed with the Center for Medicare & Medicaid Innovation (CMMI) and launched six ESCOs. Earlier this year, when the opportunity presented itself to expand, we rang the bell and added 18 more. Today, together with 800 nephrologists across the country, we manage the total cost of care for around 26,000 Medicare patients with ESRD. CMMI recently posted the year 1 results for the original 13 ESCOs and remarkably all 13 generated savings for CMS. Let me repeat that, EVERY ESCO participant saved money for CMS and the US taxpayer. To my knowledge that’s the first time every participant in a new payment model managed to move the needle. Modern Healthcare recently compared the year 1 success of the ESCO model of care with some of the more familiar models CMMI is testing. Check out the graphic below to see how the ESCO compares with Pioneer and Next Gen ACOs:
Imagine what we will see with 37 ESCOs this year.
Working collaboratively with our nephrology partners, we continue to harvest insights that improve the quality delivered to this population, while lowering their cost of care. The folks at CMMI have been a pleasure to work with and we believe the ESCO model is a step in the right direction. But the model has several warts. My colleague Dr Frank Maddux and I recently shared our thoughts about the ESCO program. Programmatic challenges that will prevent the ESCO model from achieving widespread and sustainable success include the following:
- It’s a shared savings model. All 13 original ESCOs began investing in infrastructure to support care coordination over 2 years ago. A couple of weeks ago, we received our share of the savings we generated in 2016. No one that I know will play this type of game long term.
- Transplants are ignored. Sure, we are adding a pay-for-reporting transplant measure or two in 2018, but transplant is otherwise ignored.
- Late stage CKD is ignored. Granted as nephrologists we recognize the continuum of care that connects CKD and ESRD, but addressing this continuum is not fostered by the ESCO.
In spite of these flaws, we are learning a lot, but the model is not sustainable. What’s the answer?
PATIENTS
The answer is the Dialysis Patient Access to Integrated-care, Empowerment, Nephrologists, and Treatment Services (PATIENTS) Demonstration Act, thankfully shortened to The Dialysis PATIENTS Demonstration Act. Recently introduced in both houses of Congress, PATIENTS enjoys bicameral and bipartisan support. And why not? Established through consultation with the broader renal community, PATIENTS has harvested the best of all the programs that have come before it. It’s a hybrid between the ESRD Medicare Advantage C-SNP and the ESCO, combining the best of both programs, while excluding the flaws each program possesses alone. It continues to foster the collaboration between nephrologist and dialysis provider that we see in the ESCO; it provides a funding mechanisms that does not require participants to wait a couple of years to be paid for their efforts; it allows an organization to design and deploy benefits that specifically target the needs on the ESRD population; and it creates a much needed focus on both CKD and renal transplantation. And what’s more, PATIENTS provides the patient with choice. Unlike the ESCO model where CMS rules dictate which patients are in the model (the patient cannot step out of the ESCO), the program established by the Dialysis PATIENTS Act provides the ESRD beneficiary with the option to opt out of the program and return to traditional fee-for-service Medicare.
Next steps
So, what’s next? Well as you may recall from that civics class you took in middle school, when the bill in both houses of Congress receives enough traction it will come up for a vote, likely attached to additional legislation. Today the bill has a growing number of sponsors in both houses of Congress, but of course, there’s always room for more. Historically I am not a letter writing kind of guy, and I tend to fly under the advocacy radar. But this time it’s different. This is a once-in-a-lifetime opportunity. So, yes, even I have stepped up to the plate because this piece of legislation is that important. It’s important to nephrologists. It’s important to dialysis providers. But most importantly, the patients we care for need this. PATIENTS will allow us to do remarkable things for the patients we serve. It truly is the culmination of all of the things that have come before it.
What do you think about the PATIENTS Act? Do your patients a favor and let those who represent you in Congress know how you feel. You can do that very easily here. A dozen shopping days left leaves plenty of time for you to stop what you are doing and act right now. Provide your PATIENTS with an early holiday treat. They deserve it.
Happy Holidays!
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Image from www.canstockphoto.com




RG says
Terry,
Do you see the ESCO program sun setting like the M.U. program? That is, do you think the ESCO will be a footnote one day and merge into the Patient Act?
Thanks,
RG
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Great question RG. The ESCO program was originally conceived as 3 year “experiment” with the option for 2 additional years. Should CMMI “exercise” that option, CY 2020 would be the final year of the ESCO program. Short of that, nothing is written in stone! I certainly do not have a crystal ball, but that’s never stopped me from contemplating the future. Should the PATIENTS Act come to fruition (which I and virtually every other member of the renal community hope happens), I think there are several possibilities. One possibility is that PATIENTS would coexist in a world that included the ESCO (or more likely “Next Gen” ESCO). The other very real possibility is the folks at CMS would create a glide path that would seamlessly transitioned ESCO patients into an Integrated Care Organization within PATIENTS in markets where such an opportunity exists. So much for the crystal ball, the real work is to move PATIENTS down the legislative path. Thanks for the comment RG!