 Do you believe in left- and right-brain dominance theory? In popular culture, left-brain thinkers excel in math and logic and right-brain thinkers are more creative and visual. Left-brain folks are more logical, analytical, and objective, and right-brain folks are more intuitive, thoughtful, and subjective. If true, then you have been exercising your left brain lately in thinking about MACRA and MIPS, which requires a lot of addition, subtraction, and various complex, confusing calculations. This week let’s take a left-brain break and talk about patient engagement. Expect a burst of happiness from your intuitive, emotional, visual right brain!
Do you believe in left- and right-brain dominance theory? In popular culture, left-brain thinkers excel in math and logic and right-brain thinkers are more creative and visual. Left-brain folks are more logical, analytical, and objective, and right-brain folks are more intuitive, thoughtful, and subjective. If true, then you have been exercising your left brain lately in thinking about MACRA and MIPS, which requires a lot of addition, subtraction, and various complex, confusing calculations. This week let’s take a left-brain break and talk about patient engagement. Expect a burst of happiness from your intuitive, emotional, visual right brain!
What’s the difference between engagement and experience?
Let’s first distinguish patient engagement from patient experience. In a recent NEJM Catalyst blog post, Adrienne Boissy outlined key differences. She notes that an experience is about something happening to you and how you respond to it while engagement is about interacting with something or someone. In healthcare, patient or “people” engagement includes participation in your own health, partnering with a clinical team, engaging with a healthcare system, and/or interacting with a technology. Engagement is active. In her catalyst post, Ms. Boissy identifies features of patient engagement and patient experience in this way:
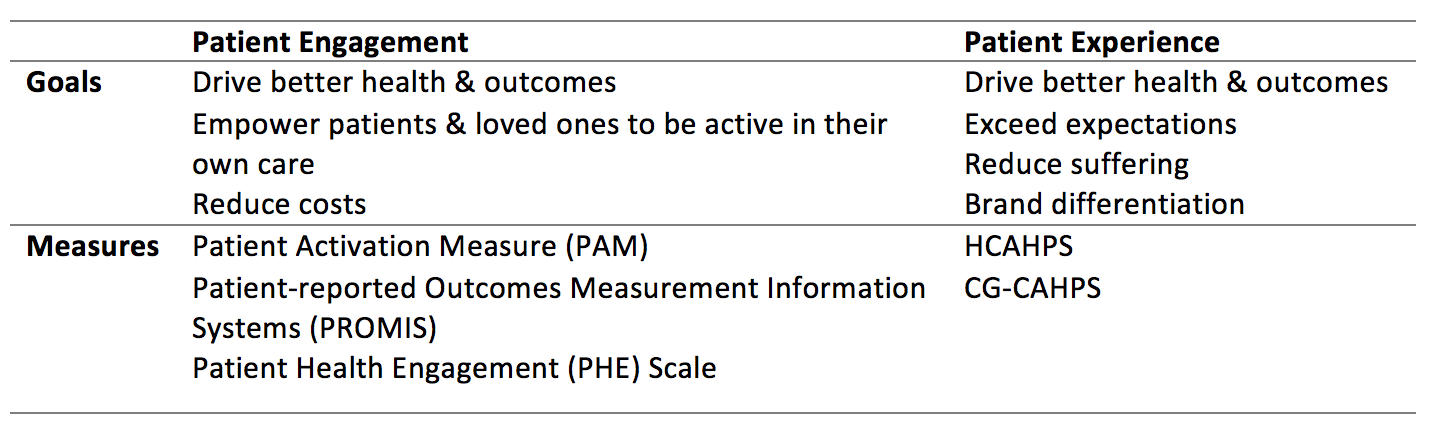
Most of us know about patient experience from HCAHPS or the Hospital Consumer Assessment of Healthcare Providers and Systems. Outside of the hospital setting CG-CAHPS or the clinician and group consumer assessment has been required for large, 100+ practice groups in PQRS. CG-CAHPS has now been re-engineered as MIPS CAHPS. Eligible Clinicians with group reporting in MIPS performance year 2017 can volunteer to administer the MIPS CAHPS survey, which is identical to PQRS CAHPS. MIPS CAHPS can count as a high-priority patient experience measure in the MIPS Quality performance category or as a high-weighted activity in the MIPS Improvement Activities performance. To participate in MIPS CAHPS groups must register with a CMS-approved vendor by June 30, 2017, and the survey is administered between November 2017 and February 2018.
Patient engagement is about participation and partnership, not consumer assessment, and it is essential for a highly functional healthcare team, with the patient as an active team member. Recent articles highlight the role technology plays in making it possible and feasible for patients to be “equipped, enabled, and empowered” as part of the healthcare team. Digital health IT supports patient engagement with tools like wearable monitors and software applications (apps) that support continuous self-monitoring, behavior change, education, and communication between patients and the healthcare team. Including patients in the design of this new technology improves the likelihood of delivering tools that are relevant, engaging, usable, and effective in patient engagement. Sometimes engaged patients bypass formal digital tool development and start grassroots IT projects, often using social media to connect with peers and disseminate ideas and innovations.
How engaged are patients today?
Far and away, most patients don’t fall into this activated e-patient group. University of Michigan researchers evaluating the impact of mobile healthcare apps describe 3 groups of patients at different stages of engagement:
- Least activated patients may have health literature challenges and/or social barriers to care. Apps that benefit this group of patients will offer health education, healthcare reminders, and general healthcare information.
- Moderately engaged patients are often already tracking health data, so they need digital tools to visualize and summarize data, receive “next step” guidance based on the data, and tools to connect to family and healthcare providers to support ongoing care.
- Highly engaged patients will look to healthcare apps for peer support through social media and for motivational challenges which may involve gamification with incentives and rewards.
Published in 2016, the Michigan research evaluated patient-facing, health-related apps for chronic diseases, including kidney disease, that are available in the Apple iTunes store and Android Google Play. This research included a rating system for the apps based on the app description, online ratings and reviews, and current updates. Out of 1,046 healthcare-related apps only 43% (n=161) of the iOS apps and 27% (n=152) of the Android apps were rated to be “possibly useful”, so there is still a lot of room for improved health app innovation.
Why the focus on engagement?
Patient engagement is highly desirable since it is associated with better clinical outcomes including quality of life, functional independence, and decreased hospitalization. Digital technology enables patients to actively contribute personal data in a dynamic and continuous way as part of the healthcare team. Good healthcare apps facilitate personal insights that can improve healthcare behaviors and support connection to others who are managing similar healthcare problems. In addition, healthcare teams can leverage technology to include patients as active team members with a shared sense of purpose and an equal voice.
Patient engagement is after all a blend of empowerment and measurement, relationship and action, insights and data. It’s a blend of right- and left-brain functioning together, which makes sense.
Right-brain, left-brain theory originated with neuropsychologist and neurobiologist Roger W. Sperry who won the Nobel Prize in 1981. Dr. Sperry studied patients who had undergone “split-brain” surgery, dividing the corpus callosum to treat epilepsy. After this procedure, which disrupted the connection between the right and left hemispheres, patients exhibited some lateralization of function. For example there is some lateralization of language between the right and left hemispheres. Both hemispheres are involved in language, but in different ways. Today it is well known that both hemispheres dynamically communicate and collaborate to provide full function and that people are not either right or left brained.
How are you using your brain to support patient engagement in your practice? Please leave us a comment.
 Dugan Maddux, MD, FACP, is the Vice President for CKD Initiatives for FMC-NA. Before her foray into the business side of medicine, Dr. Maddux spent 18 years practicing nephrology in Danville, Virginia. During this time, she and her husband, Dr. Frank Maddux, developed a nephrology-focused Electronic Health Record. She and Frank also developed Voice Expeditions, which features the Nephrology Oral History project, a collection of interviews of the early dialysis pioneers.
Dugan Maddux, MD, FACP, is the Vice President for CKD Initiatives for FMC-NA. Before her foray into the business side of medicine, Dr. Maddux spent 18 years practicing nephrology in Danville, Virginia. During this time, she and her husband, Dr. Frank Maddux, developed a nephrology-focused Electronic Health Record. She and Frank also developed Voice Expeditions, which features the Nephrology Oral History project, a collection of interviews of the early dialysis pioneers.
Photo from www.canstockphoto.com




Leave a Reply