
Have you ever wondered how Medicare decides how much to pay for an outpatient office visit? Or the monthly capitated payment we receive for caring for ESRD patients? At a very high level, the process goes something like this:
- The American Medical Association routinely convenes a committee called the RVS Update Committee (RUC).
- The RUC advises CMS about the “relative value” of one service compared to another and in this fashion has created a numerical value for every CPT code. For example, the value of 99213 (level 3 office visit for a patient you know) is lower than the value of 90960 (MCP payment for patients 20 years and older with 4 or more visits during the month).
- CMS typically accepts the recommendations the RUC has made for these relative value units (RVUs).
- Every year Congress approves a conversion factor (CF) which is $34.6062 for CY 2022.
- The fee schedule is determined by multiplying a CPT code’s RVU by the prevailing CF that year.
There are a number of nuanced details I have left out of the sequence above, but that’s the basic approach today.
Some years ago, there was another very troubling step in this process. The sustainable growth rate formula (SGR) was a complex factor that was created to ensure payments to physicians did not go through the roof over time. But as the years went by, it became clear the SGR, as legislated, did not jive with reality, and so every year Congress had to swoop in at the end of the year and pass a “doc fix” in order to prevent 20% cuts to the Medicare physician fee schedule (PFS). The solution to the SGR debacle was the establishment of the CMS Quality Payment Program via the MACRA legislation in 2015.
QPP
The quality payment program launched in 2017 and effectively created two swim lanes for physicians caring for Medicare beneficiaries:
- The Merit-based Incentive Payment System (MIPS): A budget neutral program that adjusts your future Medicare professional fee schedule (PFS) up or down based on your score across four specific categories.
- Advanced Alternative Payment Models (AAPMs): Payment models operated by CMMI which invite providers to take financial risk.
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) legislation passed with overwhelming bipartisan support. Of note, the supporters of this piece of legislation clearly preferred that providers select the AAPM swim lane. To make it more attractive, they created some financial carrots for those AAPMs determined to be what are called Qualifying Participants (QPs). The attractive carrots for participating in an AAPM and achieving QP status include exclusion from MIPS during the performance year (2022) and collecting the 5% “MACRA” bonus in the payment year (2024).
Qualifying Participants (QPs)
So, what is a QP? The QP designation is applied to all participants in an Advanced APM who demonstrate that either a significant amount of the eligible Medicare beneficiaries cared for by the providers in the program are actually in the program. Or alternatively a significant amount of model participant’s Medicare professional fees for those eligible for the model are collected from Medicare caring for beneficiaries aligned with the model. It can be a bit difficult to wrap your head around but think about it like this; Medicare is not going to reward you for participating in an Advanced APM if only a small percentage of the Medicare beneficiaries you care for who are eligible for the model, are actually in the model. How they calculate QP status is a story for another day, but suffice it to say, the ESCOs that many of you participated in the past earned the QP status each year, and we have every reason to believe the same will be true for Comprehensive Kidney Care Contracting (CKCC) and Kidney Care First (KCF) (with the exception of graduated 1 CKCC which is not an Advanced APM).
2023 and Beyond
Many of you are familiar with the story to this point, but what comes next may not be clear to you and was not clear to me until my colleagues and I recently had a chance to speak with some of the folks at CMS who are substantially involved with the quality payment program. They were extremely helpful in solidifying our understanding of what comes next.
The first point to make clear, is MIPS is here to stay. MIPS will always be a budget neutral program (i.e. there will be as many providers with a favorable adjustment to their future fee schedule as there are those with unfavorable adjustments). As such, one could make the case that administrative burden aside, MIPS will become more challenging as the years go by.
The second point is that 2022 is indeed the last year of the 5% MACRA bonus (which will be paid in 2024). As some of you may have heard there is an effort underway to convince Congress to add one more year to the 5% bonus plan, but do not assume that QPs in and AAPM in 2023 will receive a 5% bonus in 2025. That’s not in the existing legislation.
The third point is that QPs in an AAPM will continue to be excluded from MIPS during the performance year. And as noted above, MIPS is not getting easier. An exclusion may not be the eye candy we have seen with the 5% bonus, but as my father used to say, it’s better than a sharp stick in the eye.
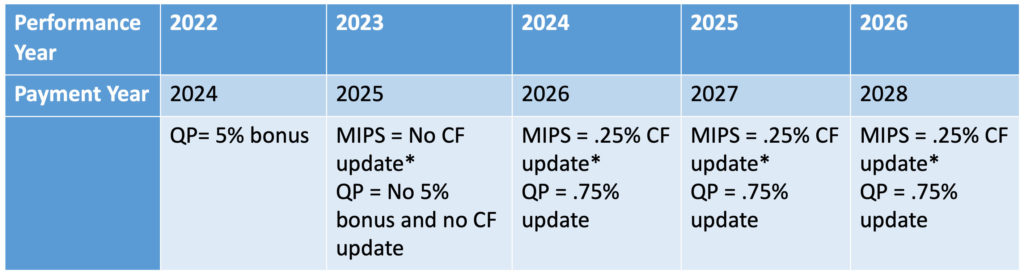
The final point to be made is perhaps the most important one. In performance year 2024, the swim lane you are in will directly impact what is referred to as an “update” to the fee schedule conversion factor mentioned above. If you are in the MIPS track during 2024, the CF will increase by 0.25% for 2026. If you are in an AAPM that achieves QP status in 2024, the CF will increase by 0.75%. As it stands today, that CF update differential will continue year after year which effectively has a compounding effect in favor of those in the AAPM swim lane. The impact of this information is displayed in the table below.
Summary
So how should I think about this as a nephrology practice? For those of you in an AAPM, like CKCC or KCF during CY 2023, assuming your model achieves QP status which I believe is a very good assumption, you will escape MIPS in 2023. If you continue to participate in CY 2024 and again achieve QP status, you escape MIPS in 2024, AND your 2026 Medicare PFS will effectively be 0.75% higher that what it would have been by simply using the CF Congress published for the year.
Your colleagues in MIPS? They will continue to compete with all types of physicians across the country in a budget neutral program which is designed to get harder as time passes. And if they are in MIPS during CY 2024, their baseline PFS will be a half of a percentage point lower than yours. I don’t know about you, but this strikes me as an easy choice.
We hope this information brings a little clarity to what at times can be a very confusing issue. We will continue to keep tabs on the future aspects of the quality payment program’s intersection with value based care.

Terry brings 28 years of experience in nephrology and value based arrangements. He splits his time between two roles, first as a Co-Chief Medical Officer of InterWell Health and also as Chief Medical Officer of Fresenius Medical Care North America’s Integrated Care Group, a division with over $6 billion of medical spend under value based arrangements.


Leave a Reply