 Summer is fading fast and before long Fall will be upon us, which means 2014 is not far off. Yet it seems like only yesterday we were discussing the Stage 1 objectives in this blog. Time does indeed fly.
Summer is fading fast and before long Fall will be upon us, which means 2014 is not far off. Yet it seems like only yesterday we were discussing the Stage 1 objectives in this blog. Time does indeed fly.
Those of you who started your meaningful use journey early are probably already beginning to plan for next year and dig into the Stage 2 objectives. Over the next several weeks we’ll attempt to unpack what lies ahead on the meaningful use highway. As with every journey, we need to begin with some basics.
2014
The first thing to notice is the name of the game has changed ever so slightly. While it is common to toss around the phrases Stage 1 and Stage 2, it is very important to recognize that ONC has created a new certification path (some might say, a gauntlet). The new badge of honor is officially referred to as “2014 Edition Certification.” Whether you are pursuing the Stage 1 objectives or the Stage 2 objectives in 2014, you must use an EHR that possesses the 2014 edition certification. The 2011 edition expires on 12/31/13. ONC will continue to maintain a list of certified records on the CHPL. The list of complete 2014 edition certified EHRs is short today, but will certainly grow by year’s end.
Reporting period
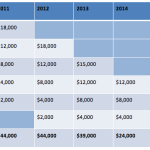
Another change is creating more than its fair share of confusion: the reporting period for 2014. With rare exception, providers will select a calendar quarter in 2014 and report the appropriate meaningful use objectives based on what transpired during those three months. In plain English, this means those of you facing the Stage 2 objectives in 2014 and those of you who reported the Stage 1 objectives for the first time in 2013 will select one of the four 2014 calendar quarters as a reporting period. Your choice will depend on many things, but bear in mind next year is not one that will smile on the procrastinators among us. Remember the 4th quarter of next year heralds the beginning of the transition to ICD-10. I don’t know about you, but facing the ICD-10 transition along with the challenges of the meaningful use framework is something I would avoid if at all possible!
Although the calendar quarter will be the most common reporting period next year, there are a couple of exceptions worth noting:
- If 2014 is your first year to participate in the meaningful use program, you still are afforded the opportunity to select any continuous 90-day period during the calendar year. The caution about the ICD-10 transition continues to apply in my view, but perhaps more importantly is the fact that 2014 is the payment adjustment reporting period for the 2.0% penalty CMS intends to levy in 2016 upon those deemed not to be meaningful users. If 2014 is your first year, make sure you demonstrate meaningful use by September 30, as the attestation deadline for first-timers who wish to avoid the 2016 haircut is October 1, 2014.
- A few nephrologists qualify for the Medicaid path to meaningful use. During the first year for Medicaid, a provider may simply attest to the fact that he or she is adopting, implementing or upgrading to a certified EHR — so called “AIU”. There is actually not a reporting period (in the standard sense of the phrase) for this group of providers and this can take place throughout 2014. Please note, however, AIU is not “demonstrating meaningful use” and Medicaid providers taking this approach will face the 2% penalty in 2016.
CQMs
The Stage 2 final rule brought a number of other changes to the program. The last one we will discuss this week relates to clinical quality measures (CQMs). Reporting quality data to CMS is a fundamental component of the meaningful use framework. In fact, ONC has incorporated reporting CQMs into the definition of meaningful use. Previously, reporting CQMs counted as one of our core objectives. That has now changed. What has also changed is the basic framework. Beginning in 2014, CMS will drop the confusing core, alternate core and menu structure that surrounded our choice of quality measures to report. In the new world, providers facing both Stage 1 and Stage 2 will report nine quality measures to CMS. Each of the 64 ONC-approved quality measures have been assigned to one of the six National Quality Strategy domains. The provider may select any nine CQMs their EHR is certified to report, as long as the nine selected include at least one measure from three of the six NQS domains.
The dog days of August will soon be in the rearview mirror as the days grow shorter and the temperatures begin to moderate. 2014 will bring a number of changes for those of you participating in the meaningful use program. Whether you qualify for one of the new hardship exceptions, or plan to face the new Stage 2 objectives, we will be here shining a light on the highway ahead. Safe travels.

Keisha Williams says
Question:
With MU stage 2…for the core objective Medication Reconciliation, can the reconciliation be done by nursing staff or does it actually have to be the physician? Nursing staff currently reviews prior medications & updates in changes during triage procedure and it would make the most sense to have them complete this reconciliation as well. KW
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
Good question Keisha,
The final rule is pretty vague about this so it is probably worth while submitting the question to ONC/CMS. Historically for the vast majority of the objectives the program does not require the provider to execute the action. Take CPOE or eRx for example, in those objectives an appropriate member of the provider’s practice can execute the action and the provider would receive credit. In a similar fashion I would expect the same for med rec, but I do not see it written down anywhere.
Thanks for the comment.