 Fall has now officially started and the leaves are beginning their annual progression through the color spectrum. As we enter the home stretch in our review of the Stage 2 objectives, let’s take a look at five Stage 2 core objectives that got their start on the Stage 1 menu. As we do so, I’d like to introduce you to a white paper recently published by CMS. The paper provides an analysis of the results ONC achieved during 2011, the first year of the meaningful use program. The analysis is restricted to those providers taking the Medicare path to meaningful use. Of interest, 57,808 eligible professionals—or roughly 10% of those eligible—successfully participated in 2011. Among this group were almost 12,000 primary care physicians and 39,000 specialists. Nephrologists fall into the latter category and I will confine my comments about this white paper to this group of participants.
Fall has now officially started and the leaves are beginning their annual progression through the color spectrum. As we enter the home stretch in our review of the Stage 2 objectives, let’s take a look at five Stage 2 core objectives that got their start on the Stage 1 menu. As we do so, I’d like to introduce you to a white paper recently published by CMS. The paper provides an analysis of the results ONC achieved during 2011, the first year of the meaningful use program. The analysis is restricted to those providers taking the Medicare path to meaningful use. Of interest, 57,808 eligible professionals—or roughly 10% of those eligible—successfully participated in 2011. Among this group were almost 12,000 primary care physicians and 39,000 specialists. Nephrologists fall into the latter category and I will confine my comments about this white paper to this group of participants.
Objectives once deferred, soon required
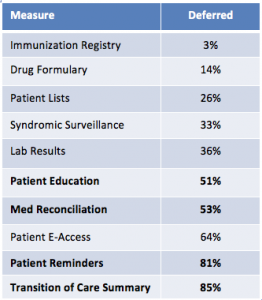
As you may recall, in Stage 1 each provider was compelled to select five of the ten menu objectives. The white paper reports the frequency with which providers selected objectives from the menu. ONC actually prefers to report the opposite, as the word “deferral” in the table below implies the percentage of providers who did not select the specific menu objective. That is to say the provider deferred that objective until Stage 2 when it appears in the Core set of objectives. (Syndromic surveillance is the lone exception as it remains on the menu for Stage 2.)
Of particular interest, four of the five Stage 2 core objectives this post covers were among those most frequently deferred in 2011. The four are bolded in the table below.
Deferral rates for Stage 1 Menu objectives
1. Incorporate Clinical Lab Results
Counted among the Stage 1 menu objectives as one of those least likely to be deferred, the lab objective moves to the Stage 2 core with very little change. The denominator remains the same—lab tests ordered by the provider during the reporting period. In fact the only thing that changes in the move to the Stage 2 core is the threshold increases from 40% to 55%. Another interesting fact from the white paper referenced above is that when specialists elected to report this objective from the Stage 1 menu in 2011, their average performance rate was 92%, well above the Stage 2 target. This hurdle should be relatively easy to clear.
2. Patient Education
A cynical man might count this objective among the few that actually deliver tangible value. Who could argue the benefits of providing educational material to our patients? This objective is unchanged as it moves from the Stage 1 menu to the Stage 2 core. Success requires that at least 10% of the provider’s unique patient encounters during the reporting period receive patient-specific education material. Note in the table above, half of the specialists reported this in 2011. The average performance for those who did report was 50%; again, well above the Stage 2 target of 10%.
3. Patient Reminders
There are a few changes for this measure in Stage 2. The denominator changes from unique patients over the age of 65 (ignoring pediatrics for the moment) to any patient with two or more office visits with the provider during the last two years. The objective is asking if at least 10% of these patients received reminders for preventive care during the reporting period, which will require workflow changes for many nephrologists. Note in the table above almost two-thirds of specialists deferred this one in 2011.
4. Medication Reconciliation
This objective looks very much like it did on the Stage 1 menu. I like to think of this as an “inbound” transition of care objective. If you are on the receiving end of a transition of care, at least 50% of the time you need to reconcile the patient’s medication list. Examples of such a transition would include seeing a patient in the office following a hospital stay, or perhaps seeing them in follow up after you referred them to a cardiologist. This is sound medical practice and I do not foresee problems for nephrologists meeting this measure.
5. Summary of Care
This one requires our attention, as it was the most commonly deferred menu objective in 2011 (labeled Transition of Care Summary in the table above). What this means to me is we have very little experience executing this objective in the wild. I tend to think of this one as an “outbound” transition of care. If you are on the sending end of a transition of care, at least 50% of the time you need to send a summary of care with the patient. Every certified EHR is capable of generating a summary of care document. Truth is, this document contains very useful information including, but not limited to, the patient’s med list, allergies, problem list, lab results, vital signs, etc. However, this gets a little tricky because there are a couple of fractions here. The 50% I refer to above is how the measure was written on the Stage 1 menu. For the Stage 2 core, in addition to sending a summary of care with the patient 50% of the time, in at least 10% of these encounters the summary of care must move from your hands to the recipient of the transition of care electronically. Your certified EHR will provide you with the tools to accomplish this, but again few docs actually elected to do this in 2011 so workflow changes will be in order.
The arrival of autumn has been accompanied by a few challenges this year. We are less than a year away from the ICD-10 transition and our Federal Government appears to be on holiday. Of course those of us at the Acumen blog won’t let you down. Enjoy the fall foliage if you can. We will be back in two weeks to finish up the Stage 2 core review.


RG says
How does the accepting doctor get the summary of care document? How do we have the accepting EMR get it electronically?
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
Different EHRs may tackle this differently, but every certified EHR must do so in a method that is compliant with the acceptable standards. We are utilizing what’s called the “Direct” standard to accomplish the exchange.