 Last week I attended the American Society of Nephrology (ASN) meeting in San Diego along with thousands of other nephrologists. The 4-day conference, with packed lecture halls and a busy convention center, was attended by a vibrant and robust international nephrology community. Surveying the crowd from the back of a full ballroom, it is hard to imagine there is a U.S. nephrology workforce issue. The ASN does not seem short of people or funds.
Last week I attended the American Society of Nephrology (ASN) meeting in San Diego along with thousands of other nephrologists. The 4-day conference, with packed lecture halls and a busy convention center, was attended by a vibrant and robust international nephrology community. Surveying the crowd from the back of a full ballroom, it is hard to imagine there is a U.S. nephrology workforce issue. The ASN does not seem short of people or funds.
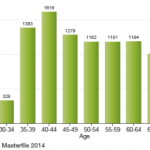
New information about the state of the nephrology workforce is now available in the recently released U.S. Nephrology Workforce 2015 Development and Trends report prepared for the ASN by the George Washington University (GWU) Health Workforce Institute. Data in the report’s executive summary confirms an ongoing disturbing trend, with an 8% drop in new nephrology fellows in 2014 and the prediction of a further drop in 2015. This decrease in the supply of nephrologists may be only one side of the story since some data suggests that the demand for nephrologists may decrease if health care delivery models continue to change.
Shortage of specialists where ESRD is most prevalent
Data presented in the ASN report illustrate that the perceived shortage of nephrologists is in part related to a mal-distribution of providers. Areas with higher numbers of ESRD patients have fewer nephrologists and a higher ratio of dialysis patients per nephrologist. This is attributed in part to the location of nephrology training programs and the fact that many nephrology fellows choose to settle and practice near where they train. Maps in the ASN report show a high concentration of nephrology training programs along the Northeastern seaboard and in large metropolitan areas. ESRD prevalence maps show high patient concentrations in the South and Midwest, in areas underserved by nephrologists today. The report notes that, “…20% of the areas with the greatest concentration of nephrologists have less than 62 people with ESRD per nephrologist, while areas with the lowest concentration have more than 105 people with ESRD per nephrologist.”
Impact of hospitalist programs and technology
The GWU research group conducted interviews and focus groups with current nephrologists to document perceptions of changes in healthcare and nephrology in this time of ACO/ESCOs, value-based purchasing incentives, hospitalist programs, and team-based care coordination. Active practitioners noted that hospitalist programs have had a dual impact on their practice. The interviewed nephrologists reported decreased hospital-based activities, such that the traditional 30% hospital, 30% clinic, and 30% dialysis care has changed to less hospital and more outpatient clinic time. In addition, hospitalist positions with higher starting salaries and shift-based work seem to be drawing internal medicine residents away from specialty fellowships, making it more difficult to recruit new nephrology partners.
While nephrologists highly value the long-term relationships they have with their outpatient clinic patients, they are frustrated by EHRs which seem to be more about billing and coding than patient care. However, some new health technology is perceived as helpful, like secure texting, which supports physician communication about patient care.
Overworked and underpaid
In the focus group one nephrologist said, “as a nephrologist, you’re underpaid and you’re overworked.” This tough combination of challenging work-life balance and comparatively low compensation in nephrology definitely seems to be part of the downward drag on attracting new fellows. There is some data about nephrology compensation in the Medscape Salaries 2015 Report. In overall physician compensation, primary care providers earn on average $195,000 while specialist annual average income is $285,000. Of 26 specialties included in this report, nephrologists ranked 18th, with an average annual patient care compensation of $243,000, while general internal medicine specialists ranked 23rd. In this Medscape survey, however, nephrology ranked next to last in “overall career satisfaction”. When asked if they had it to do over again only 66% of surveyed nephrologists would choose to study medicine and, of those, only 37% would choose nephrology.
Real demand for nephrology leaders
The GWU research for the ASN included interviews of leaders from large dialysis organizations, which covered issues regarding workforce supply and demand and use of physician extenders. Despite changing care delivery models, the dialysis industry leaders noted that they expect to have a demand for trained nephrologists. They noted that in an integrated care environment nephrologists may have more of a team-leader role, utilizing members of the multi-disciplinary team to deliver patient-care services. Physician extender use in nephrology today is largely focused on dialysis rounds, but in the future extenders are likely to play a larger role in CKD, coordinated care, and end-of-life care services. Nephrologists will likely have greater responsibilities as a team leader in and out of dialysis facilities, with population health management to meet quality care targets in value-based reimbursement models.
The 2015 ASN Workforce report provides a data-supported analysis of the current and future state of the nephrology workforce, and further research is planned. Is your nephrology practice changing for better or worse? Is your practice impacted by hospitalists? Would you practice nephrology again if you had it to do over again? Post a comment and weigh in.
 Dugan Maddux, MD, FACP, is the Vice President for CKD Initiatives for FMC-NA. Before her foray into the business side of medicine, Dr. Maddux spent 18 years practicing nephrology in Danville, Virginia. During this time, she and her husband, Dr. Frank Maddux, developed a nephrology-focused Electronic Health Record. She and Frank also developed Voice Expeditions, which features the Nephrology Oral History project, a collection of interviews of the early dialysis pioneers.
Dugan Maddux, MD, FACP, is the Vice President for CKD Initiatives for FMC-NA. Before her foray into the business side of medicine, Dr. Maddux spent 18 years practicing nephrology in Danville, Virginia. During this time, she and her husband, Dr. Frank Maddux, developed a nephrology-focused Electronic Health Record. She and Frank also developed Voice Expeditions, which features the Nephrology Oral History project, a collection of interviews of the early dialysis pioneers.


Leave a Reply