 I think it’s time to finally tackle the part of MIPS that I’ve been avoiding. It’s the category that Dr. Ketchersid deemed the overnight MACRA sensation due to its large impact on your MIPS score. It’s also arguably one of the more confusing categories to understand. Do you know which one I’m talking about? The title probably gave it away, but today we will be digging into the world of quality!
I think it’s time to finally tackle the part of MIPS that I’ve been avoiding. It’s the category that Dr. Ketchersid deemed the overnight MACRA sensation due to its large impact on your MIPS score. It’s also arguably one of the more confusing categories to understand. Do you know which one I’m talking about? The title probably gave it away, but today we will be digging into the world of quality!
MIPS composite score recap
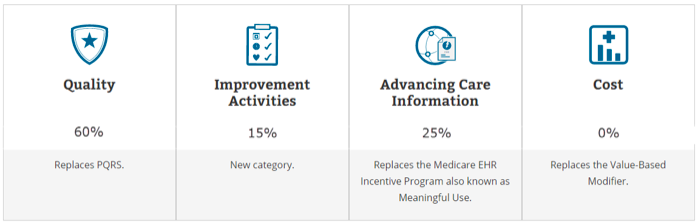
As you probably read by now, if you are a clinician in the MIPS track next year, your MIPS composite score will be made up of 4 different categories (as shown below). Notice that the quality category is worth over double any of the other categories!
In order to get a perfect 60% in quality, a clinician will need to earn a total of 60 (or 70) points.
Clinicians will earn points in the quality category of MIPS by their performance on quality measures and collecting bonus points.
Measures selection
Most clinicians must select 6 of about 300 individual quality measures (across any combination of quality domains) where 1 must either be:
- An outcomes measure or
- A high-priority measure (if an outcomes measure is unavailable)
In addition to the 6 measures, CMS will calculate (through claims data) on the “all-cause hospital readmission” measure for groups with 16 or more clinicians and a minimum of 200 cases. This measure is also worth up to 10 points. Groups below that threshold will not have this measure included.
If you cannot find 6 applicable measures, CMS will reweight your quality category based on the number of measures you are able to select. If you choose not to submit any measures at all, you will get a zero in the entire category!
Another alternative would be to report all measures in a “specialty set”. A specialty set is similar to the “measures group” concept in today’s PQRS world. Essentially CMS tried to ease measure selection by assembling sets of measures for specific specialties found under the American Board of Medical Specialties (ABMS).
If the measure set contains fewer than 6 measures, MIPS eligible clinicians will only need to report on all available measures within the set. If the specialty set contains more than 6 measures, the clinician will only need to select 6.
Sorry nephrologists, much to my dismay, there is no specialty set for you. Our beloved CKD measures group has sailed off into the sunset. Instead, you will need to dig through the full list of measures to find ones most suitable for your scope of practice.
Which patients do I report on?
Your reporting all depends on which submission route you decide to take!
- Individual MIPS eligible clinicians or groups submitting data on quality measures using QCDRs, using qualified registries, or via EHR need to report on at least 50 percent of the MIPS eligible clinician or group’s patients that meet the measure’s denominator criteria, regardless of payer for the performance period. In other words, clinicians will need to send quality data for both Medicare and non-Medicare patients.During the transition year in 2017, clinicians who do not submit at least 50 percent of their patients for each measure will receive the minimum score of 3 points per measure submitted.
- Individual MIPS eligible clinicians submitting quality measures data using Medicare Part B claims would report on at least 50 percent of the Medicare Part B patients seen during the performance period to which the measure applies. Doubt many nephrologists will go this route!
- Groups submitting quality measures data using the CMS Web Interface or a CMS-approved survey vendor to report the CAHPS for MIPS survey would need to meet the data submission requirements on the sample of the Medicare Part B patients CMS provides.
The most popular option from the list above will be the first one. You will need understand how the measure is calculated and ensure that 50 percent of your patients who meet the denominator criteria are being reported. CMS will ramp up the data completeness threshold to 60 percent in 2018.
Let’s take a look at an example for a little help:
The “Diabetes Foot Exam” clinical quality measure denominator looks for all patients (ages 18-75) with type 1 or type 2 diabetes who were seen for a specific type of visit during the reporting period. If you choose this measure, 50 percent of your type 1 or type 2 diabetes patients that meet the age and encounter requirements will need to be reported on for the performance period you select.
You will want to ensure that the tool you are using (EHR, Quality Registry, or QCDR) is tracking all of your outpatient encounters to be on the safe side. It should also be able to automatically calculate the measures you select.
In addition to all of this, you will need a minimum of 20 cases per measure. If you do not have at least 20 cases and still decide to report the measure, CMS will award you a maximum of 3 points (in 2017 only).
Quality scoring and earning points
Now that you understand how to select measures and how many patients to submit measures for, let’s examine how you will earn points for these measures. This is where things get even more complicated.
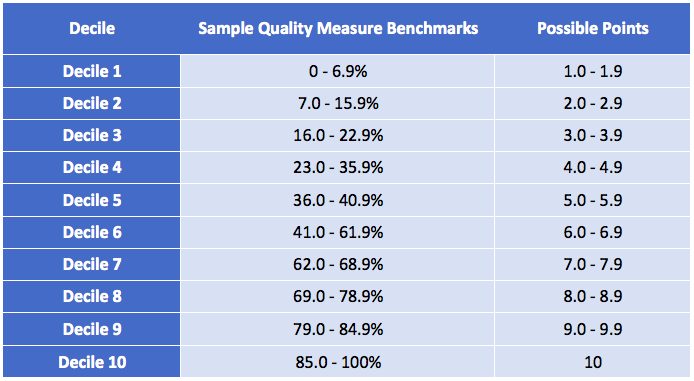
Each measure is worth up to 10 decile points. Each year, CMS will publish deciles for each measure based on national performance in a baseline period (which is two years prior to the performance period). Performance is compared and points are assigned based on the decile range in which the performance data is located, all receiving at least 1 point depending on the comparison percentage figure.
Take a look at the example below. Let’s assume it is for the “Diabetes Foot Exam” measure in which you scored a 79% during the reporting period. In this case, you would get 9.0 decile points for the measure (out of a possible 10 points).
You would go through this exercise with the remainder of the 6 measures you selected to estimate your total quality score. The benchmarks for each measure will be published prior to the performance period.
Now for those of you wanting to report on newer measures—buyers beware!
For newer measures, CMS doesn’t have enough data to benchmark in order to assign deciles. Each benchmark must have a minimum of 20 individual clinicians or groups reporting the measure in order to meet the data completeness requirement and minimum case size criteria and performance greater than 0.
Therefore, CMS will have to use data from the current performance period to create measure benchmarks. This information won’t be available until after the end of the performance period (and in turn you will not be able to predict how well you did).
To overly complicate things, in 2017 only, MIPS quality measures that do not have a benchmark will not be scored based on performance. Instead, these measures will receive a maximum of 3 points. Because of this, if you are submitting data for MIPS next year and are trying to earn incentive dollars (vs avoid a penalty), new measures may not be the way to go.
Lastly, if you are at the end of a reporting period and still have a 0 percent in some of your selected measures, report them anyway! In 2017, CMS will award a minimum of 3 points just for submitting the measure (assuming you reported on 50 percent of patients in that measure’s denominator).
Still not doing so hot? Bonus points are available!
Much like in ACI, clinicians can earn bonus points to help increase their total quality score. Bonus points can be earned 2 different ways:
- Reporting on additional outcomes/high-priority measures: Two bonus points will be awarded for every additional outcomes measure (outside of the required) and patient experience measure selected. One bonus point will be awarded for every high priority measure selected. This bonus opportunity will be capped at 10 points.
- End-to-end reporting: One bonus point will be awarded for each measure if an eligible clinician uses certified EHR technology to capture and report quality data to CMS. This bonus opportunity will be capped at 10 points.
What should you do?
Before you start selecting measures, you will need to know if your practice is participating in an alternative payment model (APM). If it is, then most likely your measures have already been selected on your behalf and your quality score will be submitted by the APM.
If you are not in an APM, choose your measures wisely. Take a look at your historic Meaningful Use performance data to see how well you’ve been doing on measures you are already familiar with. This will allow you to see where you can improve for next year. Otherwise, you could sift through the 300 measures available in the final rule to find new measures.
Some important things to keep in mind:
- Not all measures can be reported through your EHR. Some can only be reported through a registry, which could involve extra setup and interface fees
- You are competing against everyone else who reports that measure (you are not given special treatment because you are a specialist)
- Due to the transition year next year, CMS is allowing you to completely skip this category as long as you report on 1 improvement activity or the base measures under Advancing Care Information. Otherwise you can report just 1 quality measure in order to avoid a penalty as well.
Phew! There is still so much more to cover on this topic but I don’t want to nudge the monster too hard. Hopefully this is enough information to get you started—and as always, expect us to dive deeper in a future blog.
What do you think of the largest MIPS category? We’d love to hear your opinions below!
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Top image from www.canstockphoto.com


Wally Stamper says
Do you have a list of what measures CAN be reported through the Acumen EHR?
Diana Strubler says
Yes, the quality measures that Acumen will be able to report in 2017 are the same clinical quality measures we have on your Meaningful Use dashboard (with the exception of LDL – that measure is being retired next year). We are looking at a list of additional measures to also support in 2018. Thanks for reading!
Diana
Colby says
My question is regarding the 20 case minimum for reporting:
” you will need a minimum of 20 cases per measure. If you do not have at least 20 cases and still decide to report the measure, CMS will award you a maximum of 3 points (in 2017 only)”
My question is, now that there is a group reporting option available, is the 20 case minimum able to be fulfilled by the entire groups total on each specific measure, or does each provider still need their own 20 cases for each measure?