The Madness of March is behind us, culminating in the U Conn men’s and women’s basketball teams cutting down the nets on consecutive nights last week. Consistent quality performances are required to win athletic championships, and while the transition is a stretch, I’d like to devote this week’s post to physician quality reporting. I’ll focus on the existing CMS programs and try to weave them into a story that makes sense.
CMS Quality Reporting: An Evolution
From the perspective of the practicing nephrologist, quality reporting to CMS can be thought of as evolving through 3 similar and related quality reporting programs:
- The physician quality reporting system (PQRS)
- The clinical quality measure (CQM) component of meaningful use
- The Physician Value-based Payment Modifier (VBP)
Each of these programs involves reporting quality data to CMS. The quality component of the first two programs falls into the “pay-for-reporting” bucket, while the physician VBP is better characterized as a “pay-for-quality” or “pay-for-value” program. Let’s examine what quality looks like from the perspective of each program.
PQRS
The physician quality reporting system (PQRS) is the granddaddy of the group. Initially called PQRI, the program started in 2007 and is now in its eighth consecutive year. We have written about the “carrot and stick” incentive structure before. Suffice it to say that with rare exception, you are being rewarded (or penalized) for simply reporting quality metrics to CMS. The vast majority of the quality measures available for reporting are process measures, as opposed to outcome measures. For example, CMS is measuring the administration of the flu vaccine, not the occurrence of influenza. Outcome are more difficult to measure, but some would argue they should be the true drivers of quality reporting.
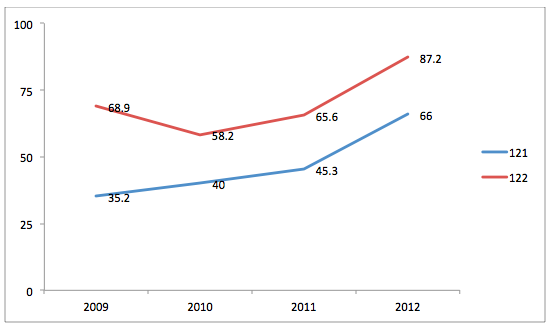
CMS recently published a brief summary of the program’s experience through 2012. Those of you suffering from insomnia may want to take a deeper dive by accessing the 3MB zip file at the bottom of the download section here. Buried in the bowels of the appendix is an intriguing view. Two of the CKD PQRS measures have essentially not changed since becoming available in 2009. Measure 121 is asking if your late stage CKD patients had a lipid profile performed in the previous 12 months, and measure 122 is asking if your late stage CKD patient’s blood pressure is controlled. Figure 1 below tracks the average performance rate for these two measures between 2009 and 2012. In my view, absent the requisite statistical analysis, performance for these two CKD quality measures has improved over time. But is this the view to consider?
Figure 1: Average performance rate (percentage) per eligible professional.
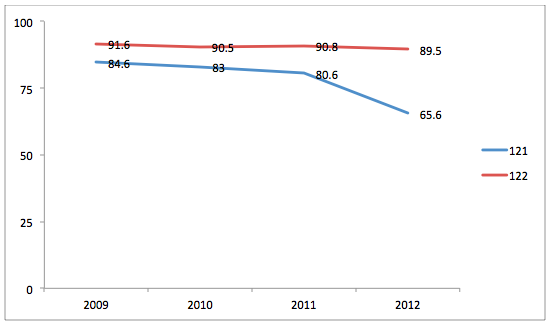
I think a more interesting view is the one displayed even deeper in the appendix (page 167 for those of you not troubled by insomnia), which is a result of CMS tracking performance trends for all measures across time by individual providers. Figure 2 looks at the same two CKD measures (121 & 122), but examines the average performance scores for the docs who reported each measure in all four years. While the numbers are small (less than 150 docs), one can probably assume all of these providers are nephrologists.
Figure 2: Average performance rate (percentage) for eligible professionals who reported the measure four years consecutively.
If indeed these are nephrologists reporting, they appear to outperform the individual measure averages (displayed in Figure 1) with the exception of measure 121 in 2012. But among this group of docs reporting the same measure year after year, there has been no improvement and perhaps a decline in quality over the course of the four years on record. Recall the incentive structure for PQRS is designed to facilitate reporting; performance, per se, is not rewarded.
MU and CQMs
2014 represents the fourth year early adopters will participate in the CMS meaningful use program. The clinical quality measures (CQM) component of meaningful use (MU) has recently changed. Regardless of whether you are reporting Stage 1 or Stage 2, you are expected to report 9 of the 64 available CQMs, and the 9 you select must cover 3 of the 6 National Quality Strategy domains. We have reviewed the CQM process before, but I bring it up here to point out the similarities between the MU CQMs and PQRS.
Reporting the CQMs is now a fundamental requirement of the meaningful use program. Of interest, your successful participation in the meaningful use program is unrelated to your CQM performance scores. As with PQRS, you are rewarded (or punished) for simply reporting the quality data. Another similarity between the CQMs and PQRS is the vast majority of the measures are process measures (not outcome measures). CMS is working diligently to align these 2 quality reporting programs, but in my view most of that will need to wait until next year. This year the reporting periods are substantially different (calendar year for PQRS and calendar quarter for MU) and this difference will create operational challenges few will likely sign up for.
Physician VBP Modifier
Last but not least is the program no one seems to be talking about. The physician VBP is truly a pay-for-quality program and one that I believe will change the way physicians are paid at the margins. This is a complex quality reporting program that essentially rewards value, where value is defined as practices delivering high quality at low cost. It’s also a budget-neutral program, which effectively means the incentives paid to those practices delivering the value are harvested by penalizing practices that deliver low quality at high cost. If this is news to you, I would highly recommend you stop what you are doing and read this quick overview of the 2015 program.
The 2015 physician VBP program is unlikely to apply to most nephrologists as only groups with 100 or more providers are participating in 2015. However, this year is basically the surveillance period for the 2016 program; every practice with 10 or more providers will be part of this quality reporting program in 2016. Note CMS casts a wide net when counting providers and included in this count are your nurse practioners and physician assistants.
The quality component of this program is very similar to PQRS, with the exception that outcomes measures are also part of the quality composite index. We will be spending more time with the VBP in this forum with future posts, but it is clear this represents another iteration in the evolution of quality reporting.
What’s next for quality reporting?
The evolution outlined above is not an accident. These pay-for-reporting programs have permitted CMS and Medicare providers to develop a broad experience with quality reporting. In 2012 for example, CMS received claims-based PQRS data for 15 million Medicare beneficiaries. Benchmarks have been established, reporting methods have been refined, and certain measures have been retired. The introduction of the National Quality Strategy has ensured that quality metrics will be equally distributed across each domain.
The Physician VBP is the latest step in this evolution and it includes a couple of important changes. First it introduces the concept of delivering quality in an efficient manner (quality as a function of cost). Second, the rewards (and punishment) are delivered at the practice level, not the individual provider level. And finally, the VBP will begin to introduce a degree of transparency not previously seen at the practice level. Transparency is more than just a buzzword these days. Who would have believed a year ago the Federal government would release provider names and their associated Medicare collections? I suspect the folks making the headlines did not.
What are your thoughts about the evolution of quality reporting?

Richard V. Paul MD says
Maybe the lack of “improvement” in checking lipid panels of CKD patients among nephrologists reflects increasing recognition of the lack of value in doing this test. The latest guidelines are also coming around to this point of view. If you are at high risk of cardiovascular events (as adult patients with CKD 3-4 are) you should probablyy be on a statin regardless of lipid levels – but if you’re on dialysis (CKD 5-6) and don’t actually have known atherosclerotic cardiovascular disease, statins have repeatedly been shown to be of no benefit. Either way, checking lipid panels and treating to some arbitrary target is a waste of time and money.
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
Great points Dr Paul. One of the concerns with quality reporting has been the nimbleness (or lack thereof) of the respective bodies supervising the reporting. The fact that these PQRS measures are virtually unchanged over time highlights this concern. As a community we need to pay close attention to this aspect of quality reporting, especially as the Physician Value-based payment modifier becomes part of our daily existence.
Thanks for your comment, Terry