 Last week our team participated in our 3rd annual Registry Kick-Off meeting with CMS. Following a couple of technical hiccups, Dr. Dan Green and his colleagues walked us through what is expected from qualified Registries this year. There are some new twists for 2011 and I would like to summarize those likely to impact the practicing nephrologist.
Last week our team participated in our 3rd annual Registry Kick-Off meeting with CMS. Following a couple of technical hiccups, Dr. Dan Green and his colleagues walked us through what is expected from qualified Registries this year. There are some new twists for 2011 and I would like to summarize those likely to impact the practicing nephrologist.
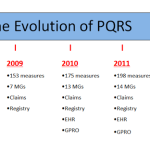
What Has Changed for 2011
- All patients reported for 2011 must be Medicare Part B beneficiaries. Yes, that’s right, unlike last year when those of you reporting a Measures Group for 30 patients only had to ensure two of those patients were Medicare Part B patients, this year all 30 must be.
- A performance rate of zero is a failure in more ways than one! Any measure that you report in 2011 that has a performance rate of 0% will not be recognized by CMS. This is a very important change. In years past, CMS was paying for reporting and ignoring performance. This year they are still paying for reporting but if you report a measure with a zero in the performance numerator, they are implying you should have picked a measure more applicable to your scope of practice. Note this also applies to those of you reporting a Measures Group. If you have a goose egg in the performance numerator for one of the measures in the Measures Group, you fail. If this rule had been in play in 2010, over 8,000 providers would have failed. The exception here is measure #1 in which the opposite holds true (performance of 100% = failure due to the odd way this measure was historically constructed).
- The CKD Measures Group (by far the most commonly reported choice by nephrologists in our experience) now has only four individual measures. Measure #135 CKD: Flu Vaccine has been dropped from the CKD MG this year. It remains as an individual measure for 2011.
- Remember 2011 is the first year you may demonstrate meaningful use. You may participate in the EHR incentive program and in PQRS concurrently.
- You may submit the e-prescribing measure through a qualified PQRS Registry as you could last year. New for this year is that successful submission of the eRx measure via a Registry is one way you may become exempt from the 2013 eRx adjustment (a 1.5% reduction in your Medicare PFS for 2013). Remember, if you take the Medicare path to meaningful use you may not collect the eRx incentive, but you may be subject to the penalty unless another proposed rule comes to fruition.
- The incentive for successful participants in 2011 drops from last year’s 2% to 1% of your total part B allowable for the calendar year.
What Has Not Changed for 2011
- Successful nephrologists will be awarded an incentive based their unique TIN/NPI pair (tax identification number and national provider identifier). Last year CMS received 2,677 TIN/NPI pairs for which they could not locate a single Part B claim for 2010. This means these providers will receive exactly $0 for participating. How could this happen? It is possible the TIN/NPIs submitted were inaccurate. (A single digit transposition in the TIN or NPI will sink this ship.) It is also possible some providers are sending the wrong NPI number to their Registry. Pay close attention to these numbers and please use your individual provider NPI—not your practice’s NPI when submitting PQRS data!
- The same five Registry reporting options are available:
– At least 80% of 3 or more individual measures for 12 months
– At least 80% of 3 or more individual measures for 6 months
– At least 80% for 1 Measures Group for 12 months (minimum 15 patients)
– At least 80% for 1 Measures Group for 6 months (minimum 8 patients)
– Report a Measures Group for at least 30 patients - As noted above, reporting the eRx measure via a Registry remains an option for Registries offering this measure. Note, however, that CMS identified 658 providers submitting the eRx measure through a Registry last year who did not have 25 eligible Part B claims in 2010. Again, these providers will not be paid. Pay attention to your TIN/NPI pairs!
In summary, Registry reporting is a fantastic way to submit PQRS and eRx data. It permits retrospective reporting and allows a degree of analysis prior to “hitting the send button.” Big changes for 2011 are the requirement to only include data for Medicare Part B beneficiaries and the new rule regarding goose eggs in the performance metric. Persistent problems with TIN/NPI mismatches require diligence by participants and their Registry alike. The incentive for successfully reporting in 2011 has dropped to 1% of your entire Part B allowable for the year— half of what it was last year—but, in my opinion, still worth the price of admission.

Leave a Reply