Last week I had the privilege of speaking to our local medical staff about CMS incentive programs. The topic of the presentation was meaningful use, but during the course of the conversation I mentioned the PQRS program and the looming payment adjustment reporting period. “How many of you have participated in PQRS?” I asked the group of 60 or 70 folks. Two hands went up. What surprised me even more was the majority of the people in the room had not heard of the program. With the table set, let’s take another look at this program.
From initiative to system
Remarkably, 2012 represents the sixth year for the Physician Quality Reporting System (PQRS). The Tax Relief and Health Care Act of 2006 gave birth to the program which was originally dubbed the Physician Quality Reporting Initiative (PQRI). The Medicare Improvement for Patients and Providers Act of 2008 (MIPPA) subsequently established the program’s permanence. Last year PQRI was renamed PQRS to reflect the program was no longer an initiative, but was here to stay.
At its core, PQRS is fundamentally a classic pay-for-reporting program. The provider submits performance data to CMS and if the provider reports successfully, CMS rewards the provider the following year by awarding a specific percentage of the provider’s Medicare Part B book of business. The performance data is captured via a series of provider-selected quality measures. I like to think of these measures as simple fractions: the denominator is the population of interest (for example, adults with late stage CKD) and the numerator represents the quality action (did the patient have a lipid panel during the past 12 months?).
Pay for reporting not quality
What separates this from a pay-for-quality program is that payment with PQRS is independent of the provider’s performance. For example, if two docs in the same practice report measure # 121 (Adult Kidney Disease: Laboratory Testing-Lipid Profile) with one doc reporting 95% of his late stage CKD patients had a lipid profile and the other doc reporting a performance rate of just 5%, both docs would receive the same 2012 incentive payment, a 0.5% bonus on their entire 2012 Part B book of business. Payment is based solely on sending the data to CMS.
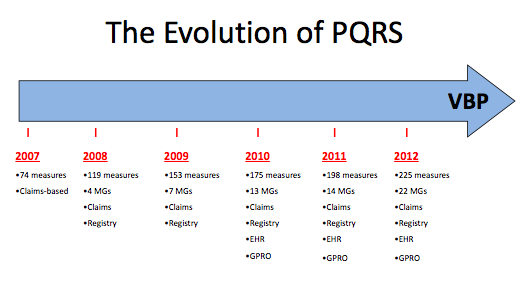
The program has grown substantially from its first year in 2007 when options were limited to choosing from 74 individual measures and reporting them to CMS by adding a series of quality data codes to your patient’s part B claim. Today there are over 200 individual measures, 22 measures groups and a wide variety of methods for reporting this data to CMS. Reporting options include the original method of claims-based reporting, the increasingly popular registry reporting option, and direct reporting from your electronic health record. Group practices may also take advantage of the Group Practice Reporting Option (GPRO).
What’s next?
Several things are just around the proverbial bend with respect to physician quality reporting. The 2011 numbers are not yet available, but in 2010, nephrologists used registry reporting more frequently than claims-based reporting for the first time in the program’s history. That trend is almost certain to continue. The rise in Registry reporting has not gone unnoticed by CMS and I suspect claims-based reporting is likely to disappear in the future. While we are making bold predictions, I think we will also see EHR-based reporting over take claims-based reporting, particularly as CMS achieves its goal of harmonizing PQRS with the clinical quality measure component of the meaningful use program.
From carrot to stick
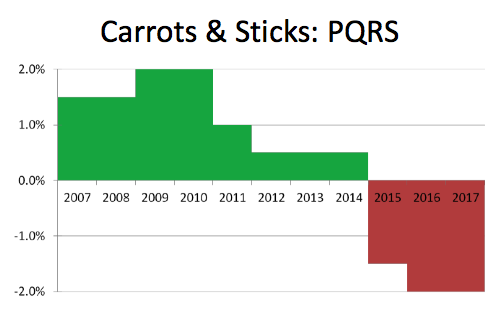
I have written before about carrots and sticks, and the PQRS program is yet another example of CMS utilizing this classic, but dated, incentive structure. 2015 is the first year a provider can be penalized for not participating in the PQRS program. Determining who to levy the 1.5% penalty upon in 2015 will be based on provider activity in 2013. As noted below, the positive incentive has declined substantially and will soon be replaced by the stick. The graph below ends with 2017, but the program is permanent and the 2% penalty today extends to all years beyond 2015.
Value-based purchasing
Earlier I made the distinction between pay for reporting and pay for performance. With the PQRS program, providers are paid the same incentive percentage regardless of performance scores. Of interest to every nephrologist is the arrival next year of the Physician Value-Based Payment Modifier (VBP). The physician VBP is a budget-neutral program which will attempt to award high quality delivered at low cost, and pay for it by penalizing low quality delivered at high cost.
As detailed in the proposed 2013 Medicare PFS, CMS intends to use the performance rates within specific PQRS measures as the basis for the quality calculation within the VBP program. The surveillance component of the program begins next year for groups with more than 25 providers, with the actual payment adjustment to follow in 2015. Providers practicing in smaller groups will become part of this program two years after the large groups start. Keep your eye on this one as it will certainly warrant our close attention in the future.
Tell a colleague
Nephrologists are by nature extremely busy folks. We practice in multiple venues and provide care to some of the sickest patients in our communities. By nature of the specialty, CMS is typically the largest payer within the nephrologist’s practice. As we continue to deliver care to our patients, we need to keep an eye on the evolution of these incentive programs and make sure our colleagues are aware of what is happening. “Marketing machine” is not a phrase that comes to mind when I think of CMS. Spread the word.

Leave a Reply