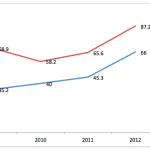
Recently I discussed changes in the Physician Quality Reporting program available for 2011. It is hard to believe this program is now in its 5th year. The old adage “time flies when you are having fun” may not apply to PQRS, but it has become an important program whether you have previously participated or not. The program is a CMS pay-for-reporting scheme that has rewarded providers for submitting quality data to CMS. In the future the reward for participating will be replaced by a penalty for non-participation. The financial incentive and penalty are calculated as a percentage of the provider’s entire Medicare Part B allowable for the calendar year. The existing schedule is noted below:

Recently, the proposed 2012 Medicare PFS was published and among other things it contains important information related to the PQRS program. Some of the PQRS highlights in the proposed rule include:
- Adding 26 additional individual measures to the existing set, bringing the 2012 total to 225 reportable measures. There is something here for everyone.
- Adding 10 additional measures groups to the 2011 offering bringing the 2012 total to 24 measures groups.
The six-month reporting period will be dropped for all providers, except those reporting a measures group through a registry. - As is the case this year, reporting a zero in the performance numerator in 2012 will be equivalent to not reporting the measure (performance goose eggs = failure to report).
- Registries will be separated into two categories: the classic PQRS registries and registries that harvest quality data directly from an her, which will be referred to as “EHR Data Submission Vendors.”
- No later than January 1, 2012, a plan must be submitted to align the PQRS program with the EHR incentive program.
As a window into this last point, next year providers categorized within NPPES as either internal medicine, family practice, general practitioner or cardiologist will be compelled to include at least one of the Meaningful Use Clinical Quality Measures (CQM) within the measures they report through PQRS. Fortunately there is overlap between PQRS and the Meaningful Use CQMs, but this will restrict the reporting options next year for the providers in these groups. Also recall last week’s post related to public reporting of quality measures through Physician Compare. It is important to begin paying close attention to the measures you report to CMS if you are not doing so today.
What are the implications for the nephrologist if the above recommendations make it into the 2012 Medicare PFS?
- The existing nephrology-facing individual measures and the CKD measures group will not change. In fact the changes highlighted for 2011 would remain in play for 2012.
- One of the new proposed measures groups is entitled “Elevated Blood Pressure.” On the surface this might appeal to the nephrologist; however, this measures group includes ten individual measures and it appears to be aimed at primary care providers.
- The requirement to align PQRS and Meaningful Use should not go unnoticed. I think we will continue to see a convergence of both programs. I doubt it is a coincidence that the penalty phases for both programs are set to begin in the same year (2015). When viewed within the context of the approaching public reporting deadlines, your selection of quality measures to report to CMS becomes increasingly important.
The public comment period for the proposed 2012 Medicare PFS is open. If you are having too much fun with PQRS and do not have time to submit a formal comment to CMS, post one here. We would love to hear from you.



Leave a Reply