Over the years, we have reviewed a number of CMS programs that sit at the intersection of nephrology and information technology. Today we start a conversation about the new kid on the block, the Physician Value-based Payment Modifier or physician VBP as it has become known. If you are in a practice with 100 or more providers, you may want to skip directly to this nicely done FAQ on the CMS website. As most nephrologists do not live in such a world, let’s take a closer look at the program.
Origins
The physician VBP is brought to you by the Affordable Care Act. While everyone was busy debating the merits of Obamacare, a small section of the ACA directed Health and Human Services (in the words of the American College of Physicians) to “develop and implement a budget neutral payment system that will employ a value-based payment modifier to adjust Medicare physician fee schedule payments based on the quality and cost of care physicians deliver to Medicare beneficiaries.”
Sounds like an idea with merit, no? As opposed to rewarding volume (standard fee for service), CMS plans to reward value delivered where value effectively equals quality divided by cost.
Who & When
The directive to HHS related to the physician VBP includes the program starting January 1, 2015, and applying to all physicians by 2017. Given that latitude, HHS has decided to start with large practices.
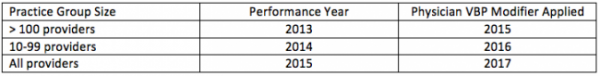
If you are in a group with 100 or more providers, the physician VBP begins in 2015. If your practice contains 10-99 providers, the physician VBP begins in 2016. The following year, all physicians are subject to the program. Similar to the meaningful use, PQRS and the e-prescribing CMS programs, the physician VBP program employs a “surveillance period” well ahead of the institution of the incentive. In the parlance of the physician VBP, the surveillance period is referred to as the performance year. The table below is intended to clarify when you will face the physician VBP.
Notice that unlike the other incentive CMS programs we have been exposed to, the physician VBP is applied at the practice level, not at the individual provider level. The rewards and the penalties are delivered at the tax ID level, not at the individual NPI level as they are with meaningful use, eRx and most renditions of PQRS. In other words, individually you may enjoy a high quality score and the “cost” of the care you deliver may be low. But if your partners are at the other end of the spectrum (low quality/high cost), you will feel their pain.
Quality-tiering
How is the payment modifier calculated? Good question and one that will require another blog post to explain. Today I will leave you with this broad overview.
Medicare beneficiaries are attributed to your practice based on a plurality of primary care services rendered to the patient during the performance year. The approach is almost identical to the attribution process in play today with many of the existing Accountable Care Organizations. What happens next is rather complex, but in a nutshell it involves the calculation of your practice’s composite cost index (Part A and Part B costs) and the calculation of a composite quality index for your practice (a combination of PQRS measures, readmission rates, and measures of acute and chronic prevention).
The devil here is truly in the detail, but once your practice’s quality and cost indices are determined, they will be compared with the national means for both quality and cost. If you are within one standard deviation of the quality composite index mean, your practice is designated “medium quality.” Likewise if your practice’s composite cost index falls within one standard deviation of the national cost composite mean, your practice is placed in the “average cost” bucket. I think you see where this is going. After CMS locates your practice’s position on the value grid, they will determine whether or not to reward your practice or penalize it. If you practice in a group with more than 10 providers (NPs and PAs are counted to determine who has 10 or more providers) your cost and quality scores are being determined by what you do this year. Based on those scores, CMS will apply the physician VBP to your Medicare Physician Fee Schedule in 2016 according to the table below:
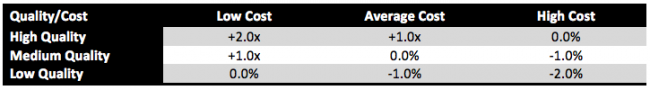
One important note, is that in 2016 only the largest practices (>100 providers) will face the downward adjustment (penalty). Smaller practices get to ease into this phase of the program. Of additional note, the “x” above is a multiplier that is determined by the amount CMS will collect from those practices they penalize. Just a reminder, this is a budget neutral program; no new money will be spent here. The rewards paid to those practices delivering value will be harvested from practices that are not delivering value in the eyes of CMS.
Implications
This program is getting very little air time today, but the more I learn about it, the more I believe this is the beginning of a significant change in the way physicians are paid for the services they provide. These are not large sums today, but I find it interesting that the maximum penalty rose from 1.0% in 2015 to 2.0% in 2016. It would not surprise me to see it climb further when the 2017 program is finalized later this year with the publication of the 2015 Physician Fee Schedule final rule.
Fee for service is not riding off into the sunset, but the physician VBP is sending a clear message, CMS intends to reward value not volume. The physician VBP begins that transition by tweaking the way physicians are paid for services provided to Medicare beneficiaries. At some point in the future, the physician VBP may become large enough that it determines how physicians are paid at the margins.
In two weeks we will unpack some of the details surrounding the calculation of the cost and quality indices. In the meantime, leave us a comment and let us know what you think about the physician VBP.

Leave a Reply