July is well underway and every summer there are some things we can always count on. Earlier this month CMS published the proposed rule that includes the 2013 Physician Fee Schedule (PFS). If you are having trouble deciding which book to bring with you to the beach, I would not include the Notice of Proposed Rulemaking (NPRM) in your consideration set. Although part thriller, part mystery, this NPRM weighs in at just over 750 pages. By definition the NPRM is proposed and open for comment, thus I do think it is useful to spend a little time with the document as it provides a view into the direction CMS intends to sail. Today let’s focus on our new friend the Physician Value-Based Payment Modifier, aka the VBP.
The physician VBP is the latest component of CMS’s stated goal to “transform Medicare from a passive payer to an active purchaser of higher quality, more efficient healthcare.” The VBP is in fact a pay for performance (P4P) program, the first real P4P program aimed directly at physicians. Unlike classic P4P programs, however, the physician VBP will attempt to quantify value. Broadly speaking, CMS wishes to reward high quality delivered at low cost. In order to do so they will define value at a high level using the following equation:
Value = Quality / Cost
Simple enough right? As usual the devil is in the details and the NPRM contains some of those that are proposed.
When does this ship sail?
The origin of the physician VBP program can be traced to MIPPA in 2008. Subsequently, in 2010, the Affordable Care Act (ACA) added additional requirements. Statute requires that this program begin no later than January 1, 2015, and that all physicians are in by January 1, 2017. So why are we discussing it today? The performance period for the first wave of providers is calendar year 2013—less than six months away.
Who is on the boat?
The proposed rule is targeting larger practices in the initial wave. Practices with 25 or more providers will be impacted in 2015, with everyone else joining the voyage in 2017. Of note, CMS has asked for comments in response to the NPRM regarding the possibility of starting everyone in 2015. CMS is dividing the large practices into those who satisfactorily participate in PQRS and those who do not. If you are in a large practice and successfully report PQRS data in 2013 and 2014, CMS proposes to set the initial value of the value-based payment modifier at 0.0%. This means the VBP will not impact your PFS in 2015. Providers in this boat will have a choice. They can do nothing and simply collect the 2015 PFS, or they can opt into the program. Opting in basically allows the provider to “earn an upward payment adjustment for high performance (high-quality tier compared to low-cost tier), and be at risk for a downward payment adjustment for low performance (low-quality tier compared to high-cost tier).”
If you practice in a large group that is not a successful PQRS participant in 2013 and 2014, the VBP modifier is set at -1.0%, which means in 2015 you would collect 99% of the 2015 PFS for services rendered that year. Of interest, the program is budget neutral and by definition will have winners and losers.
How will seamanship (quality) be measured?
I spent a little time with this until my head began to spin. (Sea sickness perhaps?) Suffice it to say CMS plans to examine and measure quality at four levels as part of this program:
- The individual physician level
- The group practice level
- The facility (hospital) level
- The community level
This first pass is focused on levels 1-3 and is largely a mix of preventive healthcare “PQRS like” measures, newly formed acute condition and chronic condition composite scores, and metrics that track hospital readmission rates.
Costs are tracked based on per capita costs incurred by Medicare, and in the “dry run” they focused on Medicare beneficiaries with four chronic conditions: COPD, heart failure, coronary artery disease and diabetes. Pharmaceutical expense (Part D) was excluded. Attribution of patients to physicians and practices involves weighted algorithms based on visits and share of E & M services (based on dollars).
Dry run
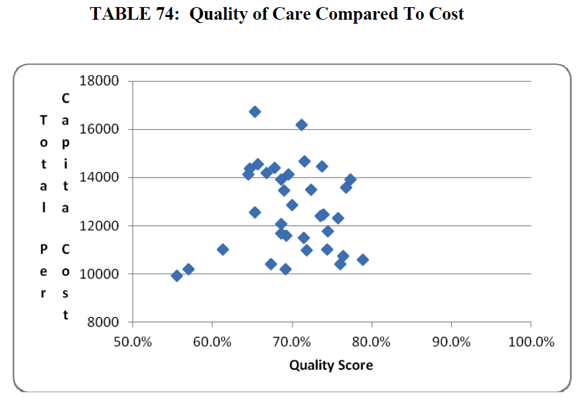
In case you are wondering how this might play out, take a look at Table 74 from the NPRM.
The 35 diamonds on this value curve represent the 35 practices that participated in the CMS PQRS GPRO program in 2010. In effect what they have done is taken the performance data those 35 practices submitted for PQRS, risk adjusted the data based on features such as socioeconomic and demographics characteristics, ethnicity and health status to come up with a composite quality score. Per capita costs were similarly risk adjusted. The plan is to divide such a graph into four quadrants and the intent is to penalize the groups that find themselves in the upper left hand quadrant (low quality-high cost) and to reward those in lower right hand quadrant (high quality-low cost).
Warning shot across the bow
Why bring this up within a blog devoted to health IT and nephrology? Largely because I do not believe this program is getting the attention it deserves. Health IT and robust clinical decision support will help you navigate to the appropriate quadrant within the value graph above. But I think the message here is to appropriately prepare for this voyage. Over 250,000 providers participated in the 2010 PQRS program. If you did not, you should consider doing so. The one percent penalty they intend to levy against large practices in 2015 as part of the VBP program will be additive to the 1.5% penalty imposed for not participating in PQRS next year. Further, some providers have gotten used to the fact that PQRS (and the meaningful use CQMs) are, in effect, pay-for-reporting programs. Many are ignoring their performance scores because they are getting paid to report, not perform. It is important for everyone to recognize the data driving the quality scores in the figure above came from the same program.
It is difficult to read the skies, but my two cents is that this ship has sailed and we need to prepare for stormy seas ahead. The CMS comment period ends September 4, but we are always available for comment. Join the conversation and let us know what you think.

Leave a Reply