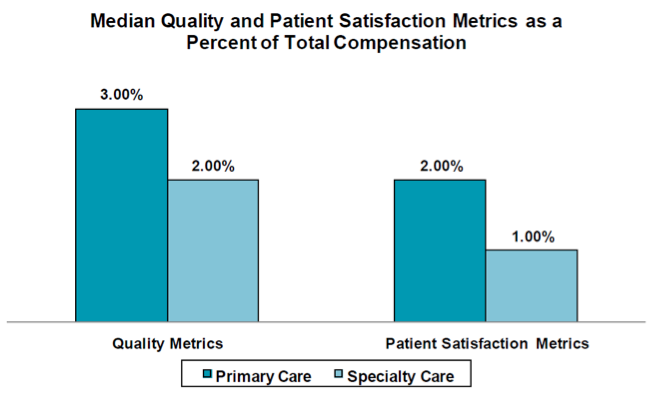
One of the messages I delivered at last week’s Acumen Users Conference was related to the importance of patient engagement in both the second stage of meaningful use and in the Physician Value-Based Payment Modifier Program. Last week I came across the following survey results chart from the Medical Group Management Association (MGMA).
The results depict a growing trend in which physician compensation is partially tied to quality and patient satisfaction metrics. While a couple of percentage points may not seem like much, remember we are very early in the game and this difference occurs, as business folks would say, “at the margin.” Economics aside, let’s take a closer look at patient engagement and its growing impact in our world.
Stage 2
The second stage of meaningful use requires substantially more “patient engagement” than the first stage. Specifically there are two new objectives in Stage 2 in which the provider’s success is dependent on the patient’s actions. These objectives include:
- Secure messaging, which requires at least 5% of the patients you see during the reporting period to send you a secure message using your certified EHR.
- Provide patients with an electronic copy of their health information, with the result (new for Stage 2) that at least 5% of the patients you see during the reporting period will either view, download, or transmit their health information to a third party.
Both of these objectives require patient engagement. Most EHRs will address these objectives with a patient portal.
PQRS and the National Quality Strategy
Previously in this blog I have mentioned the National Quality Strategy (NQS). In its current rendition, the NQS consists of six domains:
- Make care safer by reducing harm caused in the delivery of care—patient safety.
- Ensure that care engages each person and family as partners—patient experience.
- Promote effective communication and coordination of care—care coordination.
- Promote the most effective prevention and treatment practices for leading causes of mortality—clinical care.
- Work with communities to promote wide use of best practices to enable healthy living—population/community health.
- Make quality care more affordable for individuals, families, employers, and governments by developing and spreading new health care delivery models—efficiency.
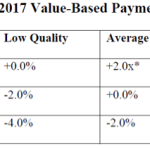
This year there are over 250 PQRS measures a provider may choose from. Each PQRS measure is assigned to one of these six NQS domains. The quality composite index component of the Physician Value-Based Payment Modifier utilizes PQRS measures and provides equal weight to the six domains. In practice this means the classic quality metrics that measure how well we did delivering clinical care to the patient are weighted equally, with metrics that measure the “patient experience.”
Historically health care providers have focused on treating patients—curing, or at least managing diseases. So called “customer service,” while not ignored, has not previously received the attention that perhaps it deserved. As the health care environment evolves, whether through medical homes, accountable care organizations, or Don Berwick’s triple aim, patient engagement is clearly becoming a much more important feature of the practice of medicine. As nephrologists, we need to recognize this and facilitate that engagement…ready or not, here it comes.

Leave a Reply