You’re probably thinking you know what’s going on in the MIPS game by now. The first year of merit-based incentive payment system (MIPS) is over and you’ve successfully attested. (We hope!) I’m sure most of you expect to be able to go on auto-drive and coast for a bit. Well, guess what? The game has changed. There is no rest for the weary, my friends!
Last week Dr. Ketchersid wrote about the ever-changing landscape we are experiencing in the healthcare arena, and this week I’m here to tell you about the ever-changing requirements under advancing care information (ACI)!
The new ACI measures
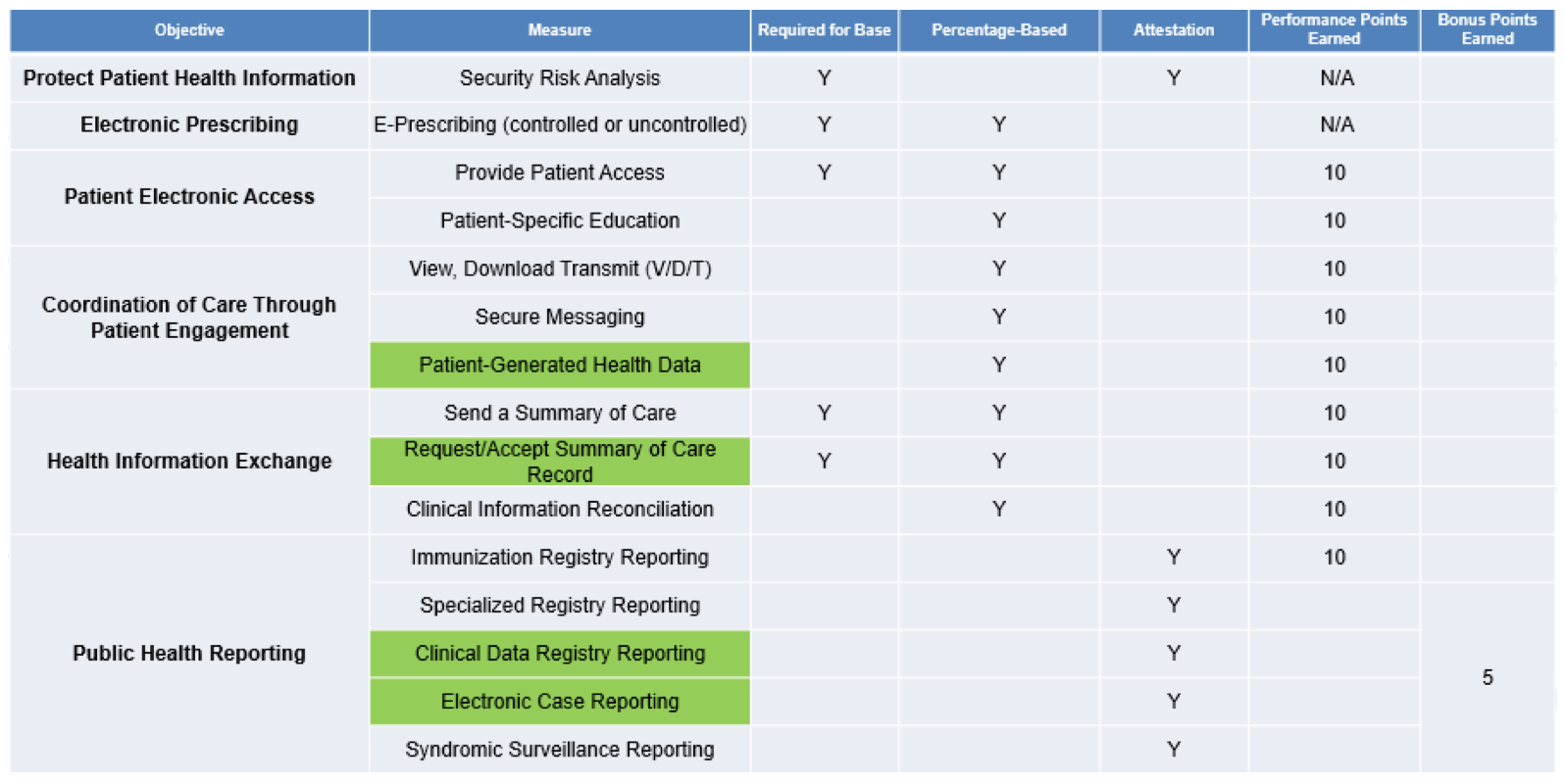
The biggest difference between the 2017 and 2018 ACI measures is the addition of 4 new measures (highlighted in green below) and a switch up of the objectives.
If you are still using a 2014-certified electronic health record, you will not see these new measures and will have to use the old measures in 2017.
If you are using a 2015-certified EHR, you will see the measures below and will also receive bonus points for this year!
The 2 new public health reporting measures (Clinical Data Registry Reporting and Electronic Case Reporting) are self-explanatory and attestation-only. I’ll leave it up to you to learn about those. I’m going to focus on the new performance-based measures: Patient-Generated Health Data and Request/Accept Summary of Care.
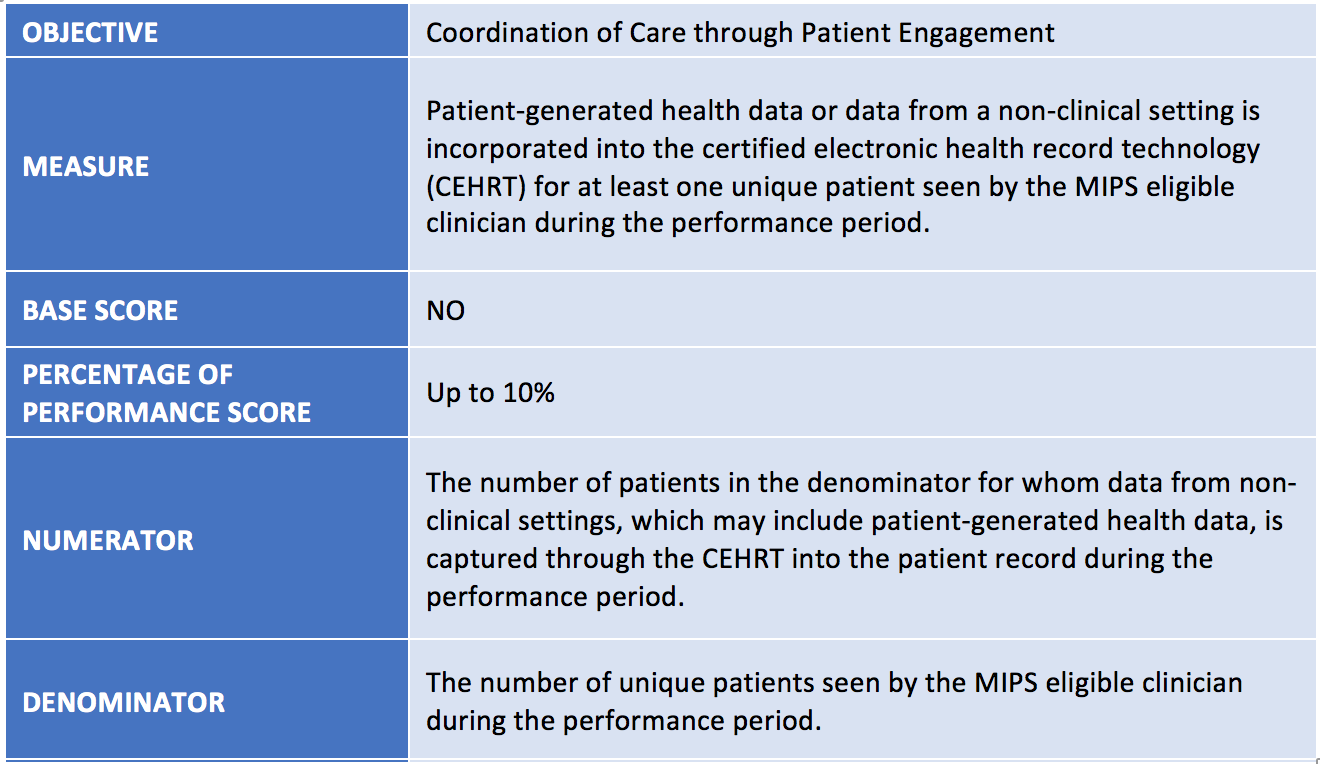
Patient-Generated Health Data
A new optional measure designed to engage the patient and create a broader care team, the Patient-Generated Heath Data measure includes incorporating health information from the patient, a patient’s authorized representative, and other care providers such as nutritionists, physical therapists, occupational therapists, psychologists, and behavioral health care specialists.
According to CMS, the types of data that would satisfy this measure are broad. They may include, but are not limited to, social service data, data generated by a patient or a patient’s authorized representative, advance directives, medical device data, home health monitoring data, and fitness monitor data. In addition, the sources of data vary and may include mobile applications for tracking health and nutrition, home health devices with tracking capabilities such as scales and blood pressure monitors, wearable devices such as activity trackers or heart monitors, patient reported outcome data, and other methods of input for patient and non-clinical setting generated health data.
There isn’t a specific way clinicians must incorporate the data, but the data cannot be related to billing, payment, or other back-of-the-house information.
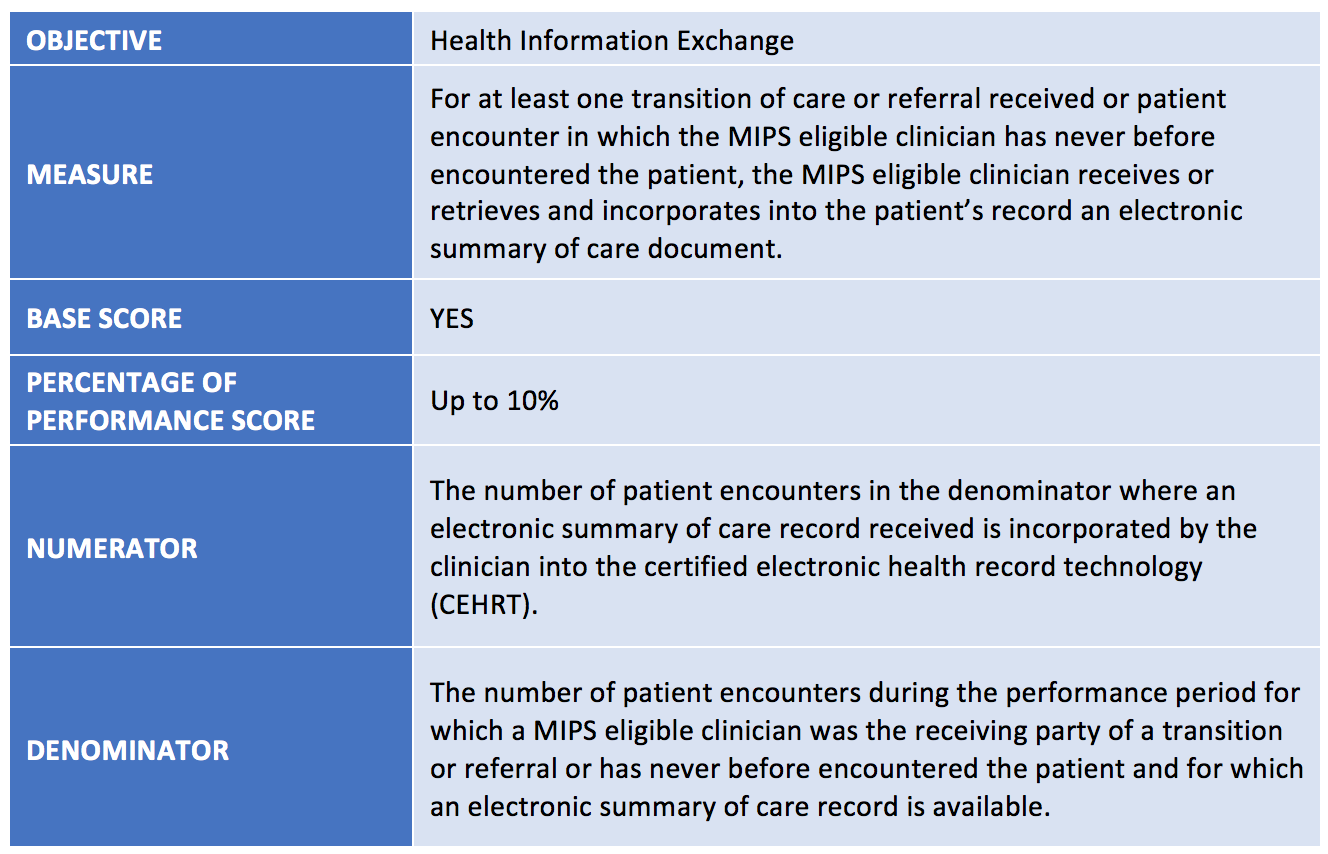
Request/Accept Summary of Care
As the new kid on the block causing the most drama, the Request/Accept Summary of Care measure is part of the “base score,” which means you must report on this measure for at least one patient otherwise you will earn 0 points under ACI.
In an ideal world, the workflow would be “automagic.” A provider would step into the exam room and his/her EHR would immediately query all outside organizations for this patient’s summary of care. The electronic summary of care would flow back into the provider’s EHR and a reconcile screen would appear. Unfortunately, the interoperability highway isn’t quite there yet.
The ONC 2015 certification program did require EHRs to create application programming interfaces (APIs) for other systems to query information, however it is a lot more complicated to implement. EHRs would need to understand the APIs of other systems, providers/patients would need to complete authorizations, and, of course, there most likely would be costs involved.
In a more realistic workflow, to meet this measure, a practice will need to request an electronic summary of care from the transferring provider (or hope the transferring provider already sent one ahead of time).
Although this measure is required, don’t fret if you don’t perform well. Remember that you can choose other ACI measures to boost your performance score.
The roadways for interoperability are still bumpy but will hopefully be paved eventually.
Modified measures
Let’s further complicate things, shall we? Not only do you have to understand the new measures I listed above, but you also have to pay attention to how existing measures have changed. This is tricky because some measures appear to be the same, but the descriptions of the measures have been slightly tweaked.
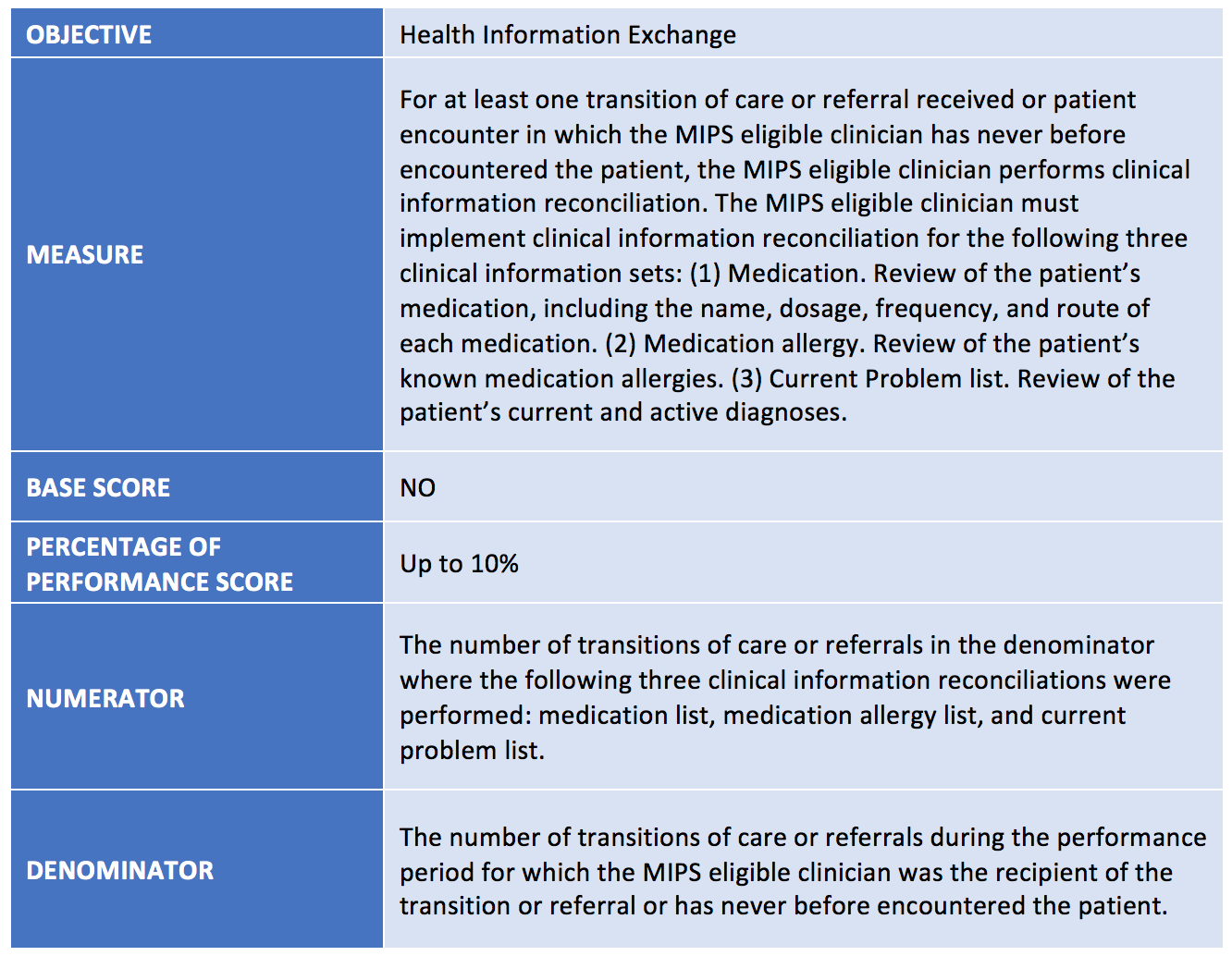
Clinical Information Reconciliation
This measure is just an enhanced version of the old medication reconciliation measure. Now, instead of reconciling medications, you will also need to reconcile medication allergies—and problems.
The Clinical Information Reconciliation measure shares the same pool of people as the new Request/Accept Summary of Care measure. You will need to perform this on all new patients and on patients who are transitioning back into your care.
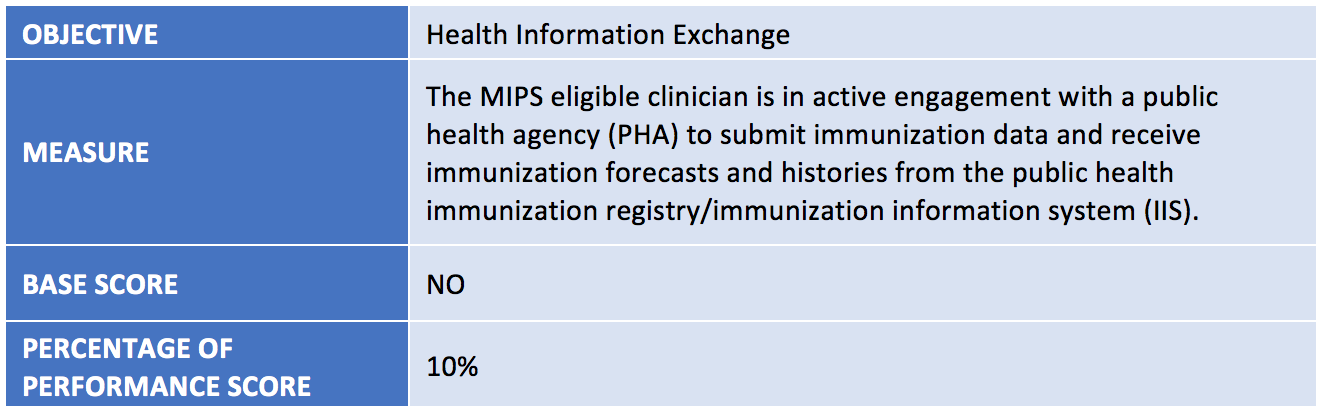
Immunization Registry Reporting
This measure is almost identical to its last version, except now clinicians will need to make sure they can receive forecasts and histories from a public health agency (PHA)/immunization information systems (IIS).
If you are using a 2015-edition EHR, you should have this capability available to you. However, it will typically require an interface between your EHR and your PHA/IIS. If you plan on reporting this measure in 2018, you will need to make sure you have this feature in place.
There’s still time!
Not only do you need to learn about these new and modified measures, you will also need to understand what workflows need to be implemented to meet these measures—and it’s already mid-April! But don’t worry. Thankfully, the ACI reporting period is only 90 days this year so you have some time to get your act together.
Take this time to peek at all of the ACI measure specifications found at the QPP resource library and also any materials your EHR vendor has provided.
For our Acumen customers, you should have received an email with reference materials, recordings, and upcoming webinar information.
Change is a good thing, right? RIGHT?! What do you think about the ACI lineup for 2018?
 Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.



Leave a Reply