The transition from summer to fall is one of my favorite times of the year. Crisp autumn days have left lawns covered in fall leaves; the college hoops season is right around the corner; and it will not be long before it’s time to carve the turkey. Last week the midterm elections turned the tables yet again inside the beltway. What this will mean for nephrologists is anybody’s guess, a guess we will leave to the pundits as we give politics a wide berth in this blog.
Today our topic is the nephrology workforce, a topic sparked by a very well-done report from the American Society of Nephrology (ASN). The ASN enlisted folks from George Washington University to take a deep dive into the current state of the nephrology workforce. If you are in a practice that’s achieved nirvana with respect to work-life balance and do not anticipate recruiting a nephrologist during the next decade, I invite you back to the blog next week. But for everyone else, the report from the ASN is worth a look.
New kids
Have you ever been at a conference, sitting around a breakfast or lunch table with colleagues when the conversation turns to the good old days? You know what I’m talking about, back when men were men (no offense ladies) and we all walked uphill in the snow to get to the hospital (uphill both ways as I recall). We were on call every night for two straight weeks and through Herculean efforts cared for the sickest of the sick. Sound familiar?
Many times those conversations lead to the current “cushy” training restrictions invoked by those with oversight of our country’s medical education programs. As a parent with a child in the midst of medical training, I have heard this before. The natural progression of conversations like this is recruitment. Many times these nostalgic reminiscences lead to conversations about trying to find a new nephrologist to join the practice. Which leads us to the ASN’s report entitled “The US Nephrology Workforce: Developments and Trends.”
Current state
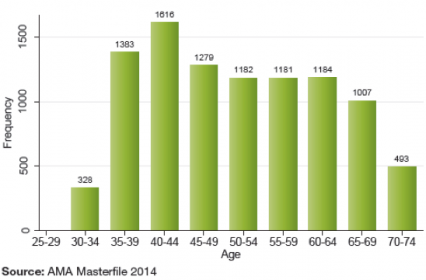
The report is well written and has many tables and graphs, a few of which are on display in this post. The age distribution chart below shows that there are roughly 9,000 nephrologists chopping wood everyday (direct patient care) and a whopping 28% are over the age of 60.
Age Distribution of Nephrologists1
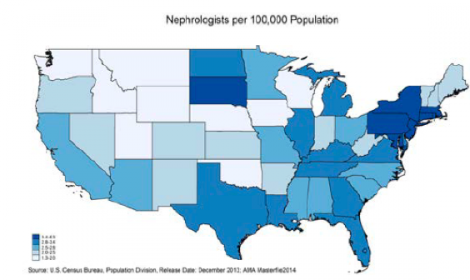
These docs are not evenly distributed across the country as the map below demonstrates. The scale is tough to read, but dark blue (Northeast) equals more docs and light colors (Iowa) fewer docs. As a point of reference, Washington DC leads the density race, with 6.3 nephrologists per 100,000 people in the district; and Iowa is bringing up the rear, with 1.3 nephrologists per 100,000 Iowans.
Number of Nephrologists per 100,000 by State, 20141
Future state
When the conversation around the table turns to recruitment, the sentiment is varied. Some practices are having success landing good candidates. For others it is more of a struggle. Part of this is also well documented in the report from the ASN.
As everyone in this space knows, there are a lot of patients with renal disease in this country and as life expectancy improves, the numbers continue to climb. Perhaps in anticipation of this growth, the number of nephrology fellowship programs rose from 128 in 2002 to 147 programs this year. In parallel, the number of renal fellows in training increased almost 50% over the last 20 years, reaching an all-time high of 930 first- and second-year fellows in 2013.
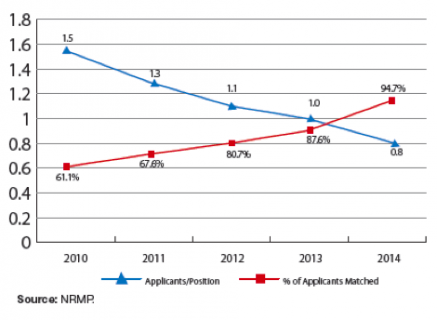
However, this is a bit of a good news/bad news story as the number of applicants for nephrology fellowship slots is trending downward. Perhaps the most troubling stat in the entire report is this one: almost 25% of the available first-year nephrology fellowship slots went unfilled in 2014. That’s right, 97 of the existing 403 positions are vacant! The direct corollary to this is that in 2010 61% of applicants to a nephrology training program matched. That number today is almost 95%, a troubling trend depicted in the graph below.
NRMP Nephrology Fellowship Match Statistics over Time1
Supply and demand
The remainder of the report does a very good job of slicing and dicing the data, pointing out a number of facts including:
- International medical school graduates (IMG) now make up 68% of the nephrology fellows compared with 42% of the physicians in an internal medicine residency (IM).
- 40% of the nephrology fellows are female physicians which is consistent with IM residents (38%).
- There’s a lack of racial diversity: Less than 4% of nephrology fellows today are African-American, while 32% of the ESRD population is African-American.
The entire report is worth your attention, but I found the last three pages very interesting. The ASN report concludes by reviewing several published surveys and papers regarding factors that influence workforce supply and demand. On the demand side, recent economic uncertainty combined with the rise in the number of nephrology mid-level providers may have dampened demand for new nephrologists. However, the fact that almost 30% of the current nephrology workforce is over the age of 60 should catch our attention. A few good years for the stock market, combined with a heavy dose of meaningful use and ICD-10, could set the stage for a spike in demand as many of our colleagues contemplate retirement.
But it’s the supply side that is most troubling to me. Our specialty no longer appears to be attractive to US medical graduates, and while we have a growing number of very talented international medical graduates, many of these folks are tethered by visa requirements that limit the geographies where they may practice. The conclusions reached in the ASN report allude to another troubling fact on the supply side of the house, one that occasionally surfaces when we reminisce about the good old days. The current internal medicine and medical school training environments establish expectations for “shift work.” When medicine residents are not allowed to work more than a specific number of hours per week or carry a census beyond a certain number of patients, the resulting environmental impact creates an expectation that is difficult to replicate in the real world of nephrology today. Couple that with the explosive growth of the hospitalist profession, a profession that mimics much of the work done during an internal medicine residency, and perhaps we should not be surprised by the number of unfilled fellowship slots.
The ASN plans to continue to address the workforce issue, and for those of you heading to the meeting in Philadelphia this week, this topic will receive quite a bit of attention. Perhaps you will bump into a colleague while you are there, and the conversation will turn to the good old days. Do you have a solution for the nephrology workforce challenges ahead? If so, drop us a comment and join the conversation.
References
1. Salsburg E, Masselink L, and Wu X. The US Nephrology Workforce: Development and Trends. Washington, D.C.: American Society of Nephrology; 2014.




David Moskowitz MD MA(Oxon.) FACP says
If 90% of chronic kidney failure could be prevented, we wouldn’t need many nephrologists at all. It would be great news for the country, but bad news for the subspecialty. The ASN won’t tell you, but I published how to prevent 90% of CKD in 2002. It’s been a very well kept secret ever since: http://www.genomed.com/images/guyot_dec09nl.pdf