Do you know how to predict your quality score in MIPS?
Starting next year, our current pay-for-reporting program (PQRS) turns into a pay-for-performance program (quality in MIPS). That means what you submit will dictate the number of bonus dollars or
penalties you could receive. In the past, clinicians could report a 1 percent in any measure without any consequence. In the MIPS world, a 1 percent in any measure could greatly hurt your ability to receive any incentive dollars and potentially take some away.
STEP 1: In order to predict your quality score, you must first decide on the six measures you want to select. Remember – one of them has to be an outcomes measure! If none of those make sense for you, you must choose another high-priority measure to take its place. Make sure that all of the measures can be reported via the same reporting method (EHR, QCDR, Claims, Qualified Registry). You can’t mix and match your reporting methods.
If you want bonus points, you should select additional outcomes or high-priority measures to round out your six. Two bonus points will be awarded for every additional outcomes measure (outside of the required) and patient experience measure selected. One bonus point will be awarded for every high-priority measure selected. This bonus opportunity will be capped at 10 points.
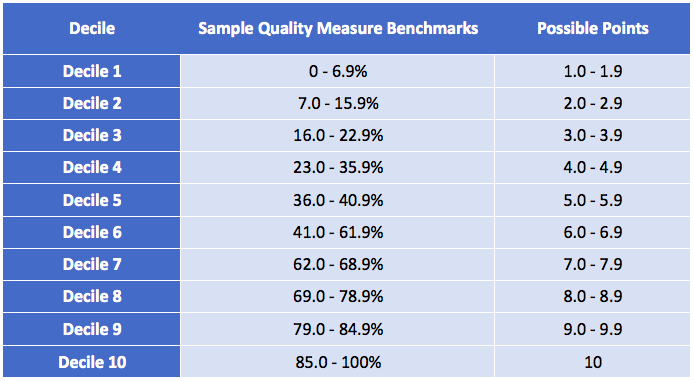
STEP 2: All right. Now that we have your measures selected, the next step is to look at the historical benchmark that CMS has published for that measure. Below is an example benchmark chart for a specific measure. If you scored a 79 percent, you would receive 9.0 points (out of 10 possible points) for this measure.
CMS will publish benchmark data prior to the start of each reporting period. That said, I haven’t seen any for next year yet.
If you decide to choose measures that you’ve never done before, then you won’t have any historical data to compare against. Also, if you choose new measures (that are less than 2 years old), CMS will not have benchmark data for those measures. Therefore, in 2017, you will only be awarded a maximum of 3 points.
STEP 3: Compare your historical percentages against the benchmarks that were published. Add up all the decile points you received for each measure. If you selected “bonus-eligible” measures, add up those potential bonus points as well! If you plan to submit each measure via your certified EHR, give yourself an additional bonus point per measure.
STEP 4: Do the following calculation! The maximum number of points will be 60 for most of you. Your maximum score cannot exceed 100 percent.
There you have it! You predicted your quality score for next year! Now, to be fair, if most of you didn’t pay attention to your quality measures (because performance didn’t matter), then your scores will probably look super low. Make a game plan on how to incorporate these measures into your workflow in order to increase your score!
Lastly, if you are in the “test path” of MIPS next year, you will not receive a penalty for your performance as long as you just submit something. However, starting in 2018 and beyond, you will want to pay attention to your quality scores.
Diana Strubler, Policy and Standards Senior Manager, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.





Leave a Reply