 Last week Dr. Dugan Maddux brought us a wonderful display of colorful images to help us digest the contents of the MACRA proposed ruling. At a high-level view, the program initially doesn’t seem like too much of a bear to tackle. If a clinician could make it through MU Stage 2, PQRS, and the VM partially unscathed, then perhaps there’s a fighting chance to do well in MIPS. However, for a clinician who works on her own or is in what CMS defines as a small practice (15 clinicians or less), the MIPS proposed ruling could hang you out to dry.
Last week Dr. Dugan Maddux brought us a wonderful display of colorful images to help us digest the contents of the MACRA proposed ruling. At a high-level view, the program initially doesn’t seem like too much of a bear to tackle. If a clinician could make it through MU Stage 2, PQRS, and the VM partially unscathed, then perhaps there’s a fighting chance to do well in MIPS. However, for a clinician who works on her own or is in what CMS defines as a small practice (15 clinicians or less), the MIPS proposed ruling could hang you out to dry.
The scandal of table 64
CMS posted (the now infamous) table 64 in the MACRA proposed rule that estimates the majority of the MIPS underperformers fall in practice sizes of 24 clinicians or less. The hardest hit will be the solo providers, with a projected 87% being hit with a negative payment adjustment in 2019. In contrast, table 64 also showed that more than 80% of clinicians in groups of 100 or more members were projected to earn a bonus.
Table 64: MIPS proposed rule estimated impact on total allow charges by practice size*
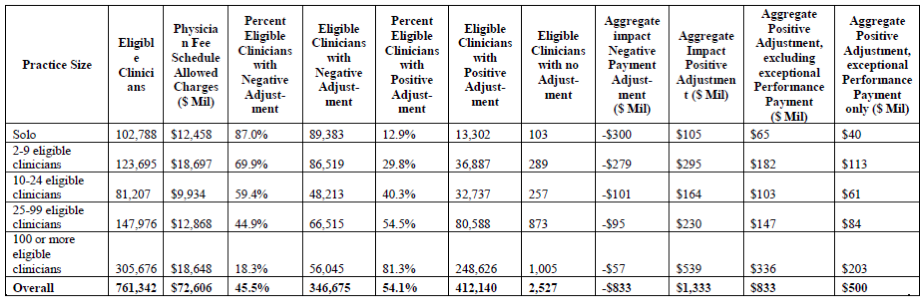 *2014 data used to estimate 2017 performance. Payments estimates using 2014 dollars.
*2014 data used to estimate 2017 performance. Payments estimates using 2014 dollars.
It didn’t take long for readers of the proposed rule to conclude that small practices are going to face major challenges in the world of MIPS. It will be very hard to compete with providers in larger practices and the resources they have in place to support the reporting burdens. Perhaps these numbers were a glaring threat from CMS that smaller practices should join an APM or slowly meet their demise?
If you ask Andy Slavitt, acting administrator for CMS, table 64 isn’t at all indicative of reality. By federal law, CMS had to assess the impact of MIPS on different clinician types. However, the only data they could go by was PQRS submission data from 2014 – where a majority of solo and smaller practices did not report. He also used this point to highlight the need to make reporting much easier.
Support for the underdogs
In response to table 64, CMS released a paper highlighting ways that CMS will provide “flexibility and support” to small practices of 15 clinicians or less and practices in a rural or health care professional shortage area. Although a majority of the paper reemphasized how the MIPS program is designed to reduce reporting burdens, there were a few points that specifically address how MACRA will try to help smaller groups and solo docs:
- Allow solo and small practices to join “virtual groups” and combine their MIPS reporting.
- Provide $100 million over 5 years in technical assistance and training.
- Reweight the “cost” category at zero if a clinician does not have enough patient volume (20 cases per measure) for any cost measures.
- Only require 2 population health measures (as opposed to 3) to be reported under the “quality” bucket.
- And, of course, a big push towards advanced APMs. In addition, those that qualify as a “medical home” and are made up of 50 clinicians or less will have unique risk standards applied compared to other advanced APMs.
The nephrologist
Now this could be a separate blog topic (and it probably will be), but another underdog in the world of MIPS is the nephrologist. When talking to solo nephrologists about the proposed ruling, a few responses were, “Why bother? I’ll just take the penalty!”
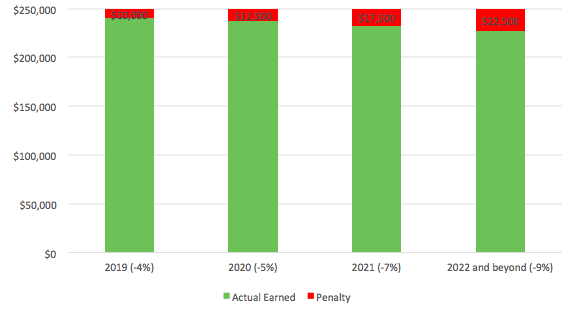
At first that doesn’t sound too bad. Let’s assume a solo nephrologist brings in $250,000 in their Medicare part B book of business. Not participating in MIPS could result in a loss of $10,000 in 2019 but could quickly grow to $22,500 per year in 2022 and beyond. Now multiply that by how many clinicians make up your practice and it adds up very fast.
MIPS Medicare Part B penalty example
CMS estimates that 42% of nephrologists (3,535) will face payment penalties in 2019. On the flip side, 59% of nephrologists (4,962) could receive some of the $37 million incentive dollars estimated.
Table 63: MIPS proposed rule estimated impact on total allowed charges by speciality: mid-point estimate*
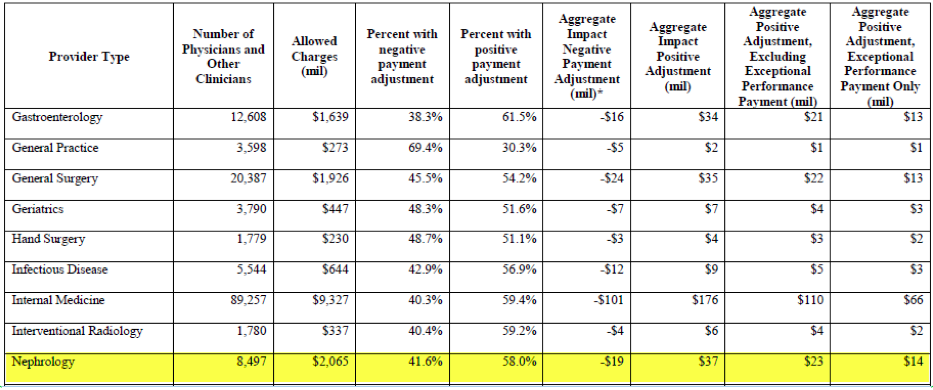 *Page 673 from MACRA proposed ruling.
*Page 673 from MACRA proposed ruling.
Perhaps you can handle taking a monetary hit, but what if your name and quality results were publicly posted and compared to your peers? By law, CMS will make publically available the results of the Quality Payment Program on the Physician Compare website. The hope of the Physician Compare website is to help patients make informed decisions. Not participating could be bad publicity.
What’s next?
It’s important to remember that all this information is still in a proposed state, which means it can all change based on public feedback. Not only will we be participating in comments back to CMS on MACRA, but you have the opportunity to comment to CMS as well. The comment period will close on June 27, 2016, and the final ruling will follow (hopefully) soon thereafter.
In the meantime, it is best to prepare as if you will be participating in the MIPS track starting next year. You can start by focusing on the quality category – it will make up 50% of your composite score and probably won’t change too much. Also start crunching numbers between the two quality payment program paths (MIPS and APMs). Dr. Terry Ketchersid provided a fun blog on the topic a couple months back. The first year of participation in this new payment world is right around the corner and – with no final ruling in hand – no minute can be wasted!
 Diana Strubler, Senior Product Analyst, Health IT Standards, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Senior Product Analyst, Health IT Standards, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.



Leave a Reply