 I had the privilege of speaking to several audiences in New Orleans last week at the annual RPA meeting. One of the popular, and perhaps controversial, topics of conversation was related to the concept of nephrologists “opting out” of meaningful use. I touched on this subject last Monday, and my perspective has not changed. However, after conversations with many of you in the Crescent City this weekend, I think it wise to revisit the issue.
I had the privilege of speaking to several audiences in New Orleans last week at the annual RPA meeting. One of the popular, and perhaps controversial, topics of conversation was related to the concept of nephrologists “opting out” of meaningful use. I touched on this subject last Monday, and my perspective has not changed. However, after conversations with many of you in the Crescent City this weekend, I think it wise to revisit the issue.
This indecision’s bugging me
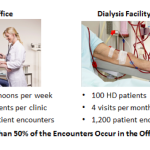
I have had the opportunity to speak with folks at ONC and CMS about this topic and it is clear to me the meaningful use framework was never intended for nephrologists. The audience is very clearly the vast number of primary care providers in this country. By some estimates, classic primary care providers out number nephrologists by a ratio that exceeds 50:1. The challenge for us of course is the encounters we have with our ESRD patients. These encounters frequently take place in a dialysis facility, and this patient population is often seen multiple times during the month.
Dialysis facilities, like nursing homes and ambulatory surgery centers, were left out in the cold, so to speak, from a meaningful use perspective. Unlike docs and hospitals, there is no financial incentive available to influence the dialysis facility’s decision to deploy a certified EHR. Further, there is no clear path for the dialysis facility to pursue if the facility indeed wished to certify their dialysis information system for meaningful use. The dialysis venue of care represents a hybrid of sorts with some work flows resembling those that take place in your office, and others resembling work flows in the hospital setting. The lack of a clear certification path for the dialysis information system is perhaps best exemplified by the list of clinical quality measures (CQMs) available within both the hospital track and the office-based or ambulatory meaningful use track. None of the available CQMs were created with the ESRD patient population in mind. The Stage 2 clinical decision support objective is attached at the hip to the CQMs, and not surprisingly, the clinical decision support rules in a Stage 2 certified EHR would be of little use to patients seen within a dialysis facility.
If I go there will be trouble
One of the concerns I heard this weekend was related to the following scenario. The docs have jumped through the Stage 1 meaningful use hoops in the dialysis facility by capturing some components of the ESRD patient population within their office based EHR (effectively duplicating data entry as many of the Stage 1 core objectives are also captured by facility staff within the dialysis information system). These docs have appropriately collected the Stage 1 incentives for their efforts, which in many cases exceeded those of their primary care colleagues, in large part because they are often personally involved with capturing all of the data within the dialysis facility. In this setting, some folks I spoke with were nervous about filing for the hardship exception I mentioned last week (more than 50% of my encounters occur in the dialysis facility, and I do not control the decision to deploy a CEHRT in that venue of care). The concern basically revolves around the issue that the doc accessed his or her office-based EHR to qualify for Stage 1, but now elects not to do so for Stage 2. Will CMS ask for the doc’s Stage 1 money back? Will CMS penalize them anyway for not jumping through the hoops in the dialysis facility (accessing their office-based EHR from within the dialysis facility and continuing to duplicate data capture) for Stage 2?
And if I stay it will be double
Based on what I have read, what I have heard on the CMS open-forum calls, and direct conversations I have had with several folks, my belief is the answer to both questions is no. I think nephrologists who have successfully attested in an environment where they needed to include their ESRD encounters to clear the hurdle established by the “50% Rule” invested substantial resources to make this happen, resources that again most other providers were not required to use. Trying to continue down this path with the Stage 2 objectives will be close to impossible.
Take CPOE for example. If you are compelled to include the in-center HD encounters within the population of patients you are reporting for Stage 2, the task is that you record your medication, laboratory and radiology orders in your certified EHR. Note the orders will, of course, also be recorded in the dialysis facility medical record or information system. This degree of duplicate data entry is untenable.
Further, from the perspective of the dialysis facility, the dialysis facility information system is the patient’s medical record. Everyone, including the nephrologist, is compelled to record information about the patient within the dialysis facility’s medical record or information system. At the end of the day, I would suggest to you the dialysis facility’s medical record, not your office-based EHR, is the source of truth for your patients receiving care in that facility.
So you gotta let me know, should I stay or should I go
I think as each of you in this position (more than half of your outpatient encounters occur in a dialysis facility) considers this hardship exception, you should carefully review the related sections within the Stage 2 final rule. Quoting directly from that rule as published in the Federal Register:
“On the other hand, there are EPs who practice at multiple locations who truly have little to no control over whether CEHRT is available at their locations. These might include, surgeons using ambulatory surgery centers or physicians treating patients in a nursing home. In these cases, the surgeon or physician likely would bear the entire impact of any payment adjustment – and such adjustment would not affect the earnings of the ambulatory surgery center or nursing home. In addition, because the surgeon or physician merely sees patients at the center or home, and does not have any other interest in the facility, we believe they would exert little to no influence over whether the nursing home, center, or other similar outpatient site adopts and implements CEHRT.”
I believe the nephrologist seeing patients in a dialysis facility is no different than the surgeon using an ASC or the physician treating patients in a nursing home-with the exception of joint venture arrangements, the scenarios are almost identical. The Stage 2 final rule goes on further to state:
“We note that we already have in place an eligibility requirement that allows for an EP to still qualify as a meaningful EHR user even if up to 49.9 percent of the EP’s outpatient encounters are in locations that lack CEHRT. Thus, our exception would apply only in the case of EPs practicing in multiple locations where the lack of control (as discussed previously) exists for a majority (50 percent or more) of their outpatient encounters at such locations, causing such EPs to not be eligible to become meaningful EHR users.”
I think the message is clear, but each of you must decide, will you stay or will you go? Give it some thought and let us know. Drop us a comment and join the conversation.

RG says
Terry,
You sure do know how to make life interesting for us. It sounds indeed like the early adopters may be at the threshold for claiming an exemption. Here are some lingering questions for you:
1. Has Acumen decided yet whether or not it will allow us to order labs in conjunction with FMC? As you know, we have monthly labs that somehow need to be counted.
2. What do you think is the best way for us to tally the dialysis unit encounters, in the way you did with your example last week? Can we use the report generator for that? Or, should we go to our practice management system?
3. For a patient that receives procrit, should we count that encounter?
4. I can’t remember who wrote that song, “Should I stay or should I go?” Do you know off hand—it is bugging me.
Thanks, RG
JY says
What about interfacing Acumen with the FMC computer systems? Could this be used to meet the requirements without doubling the documentation?
As it stands, the wireless network in Acumen lacks access to the printer, so an order generated in Acumen could not easily be printed for inclusion in a paper chart.
I am optimistic that additional integration between Acumen and the existing FMC systems would allow us to meet the Stage 2 requirements and improve documentation and patient care.
Terry Ketchersid, Vice President and Medical Officer at HITSG says
Thanks for the comments. I’ll handle the easy one first. The song is by The Clash, released in the early 80’s and perhaps their most famous tune.
Regarding procrit visits, when you are demonstrating MU, ONC has provided guidance related to nurse visits (BP checks for example). Per ONC the provider may decide whether to include these visits in their MU objectives or not, but you must be consistent (either always in or always out).
Regarding Acumen specific issues related to FMC facilities, you will certainly see increasing integration in the future, but it will be related to patient care, which oddly is of little benefit within the MU framework. Take CPOE as an example, the rules engine within the dialysis information system has enough complexity and it is in fact dynamic. Replicating this within Acumen is unlikely to occur. What’s more likely is making it easier to move between systems, but this will not assist complying with the MU CPOE objective. Again, I think a valuable option for the nephrologist to consider is the hardship exception. This permits you to continue to use the powerful tools available within the certified EHR (the interoperability parts coming in Stage 2 for example), and yet avoid the need to jump through the rest of the hoops. Next year should be exciting indeed.
Thanks for the comments.
RG says
Is there anything in terms of compliance in order to demonstrate the 50 percent rule? For example, I do believe that most nephrologists will meet this criteria, but will a back of the envelope calculation suffice, like the one you did in last week’s post? Or, will it have to be a formal precise calculation with exact numbers? It actually will be time consuming to come up with the exact numbers and codes to demonstrate that we do indeed qualify for an exemption. Complicating matters is the fact that some nephrologists do one basic visit, while a NP might do another basic visit. Of course, there is only one code that we use (1 visit vs 2 visits, vs 4 visits). Will we have to give this calculation each year, or will one year suffice?
Terry Ketchersid, Vice President and Medical Officer at HITSG says
Good question. In the audits I have seen the ask of those practicing in more than one location is simply to “provide documentation” that over 50% of your encounters occured in a venue equipped with CEHRT. It is unclear to me what they expect as supporting documentation. As you point out CPT codes are not an accurate reflection of face to face encounters in the dialysis setting. I will keep my ears open regarding folks who have been subject to an audit. Notice one of the articles in today’s news round up describes a new approach-the pre-payment audit. I have seen this happen in a nephrology practice recently.